Introduction
Gastroesophageal reflux (GERD) is a chronic disease that occurs when stomach contents flow back (reflux) into the food pipe (esophagus). At the lower end of the esophagus, where it joins the stomach, there is a circular ring of muscle called the lower esophageal sphincter (LES). After swallowing, the LES relaxes to allow food to enter the stomach and then contracts to prevent the back-up of food and acid into the esophagus.
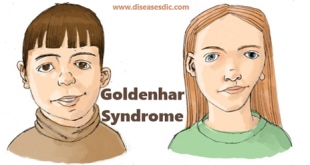
Illustration of GERD
However, sometimes the LES is weak or becomes relaxed because the stomach is distended, allowing liquids in the stomach to wash back into the esophagus occasionally in all individuals. Most of these episodes occur shortly after meals, are brief, and do not cause symptoms. Normally, acid reflux should occur only rarely during sleep.
Acid reflux — Acid reflux becomes gastroesophageal reflux disease (GERD) when it causes bothersome symptoms or injury to the esophagus. The amount of acid reflux required to cause GERD varies.
Epidemiology of gastroesophageal reflux
Western dietary habits have made GERD a common disease. Richter and associates reported that 25-40% of Americans experience symptomatic GERD at some point. Approximately 7-10% of Americans experience symptoms of GERD on a daily basis. Because many individuals control symptoms with over-the-counter (OTC) medications and without consulting a medical professional, the actual number of individuals with GERD is probably higher.
No sexual predilection exists: GERD is as common in men as in women. However, the male-to-female incidence ratio for esophagitis is 2:1-3:1. The male-to-female incidence ratio for Barrett esophagus is 10:1. White males are at a greater risk for Barrett esophagus and adenocarcinoma than other populations. GERD occurs in all age groups. The prevalence of GERD increases in people older than 40 years.
Trigger foods
Some foods are known to trigger symptoms of GERD. By keeping a food diary, you can identify your trigger foods and change your diet to reduce discomfort. Below is a list of some foods recognized to trigger symptoms of GERD and how they affect the digestive tract:
- Coffee (with or without caffeine) and caffeinated beverages relax the lower esophageal sphincter.
- Citrus fruits and juices such as orange, grapefruit and pineapple have high acid content.
- Tomatoes and processed tomato-based products such as tomato juice, and pasta and pizza sauces are highly acidic.
- Carbonated beverages (fizzy drinks) cause gaseous distension of the stomach (bloating) which increases pressure on the lower esophageal sphincter causing acid reflux.
- Chocolate contains a chemical called methylxanthine fromthe cocoa tree, which is similar to caffeine. It relaxes the lower esophageal sphincter, which causes acid reflux.
- Peppermint, garlic and onions relax the lower esophageal sphincter causing acid reflux.
- Fatty, spicy or fried foods relax the lower esophageal sphincter as well as delay stomach emptying and therefore cause acid reflux.
Risk factors of gastroesophageal reflux
- Hiatal Hernia: Hiatal hernia is associated with an increased risk for GERD. Hiatal hernia can produce a separation of the lower esophageal sphincter (LES) from the crural diaphragm, causing a weakening of the gastroesophageal barrier. The result is a degree of functional incompetence at this barrier.
- Obesity: Obesity in general, and abdominal obesity specifically, is associated with an increased risk for GERD. In a meta-analysis, being categorized as overweight (BMI >25-30 kg/m2) or obese (BMI >30 kg/m2) was associated with GERD symptoms, erosive esophagitis, and esophageal carcinoma. There is also a relationship between visceral adiposity and GERD. Presumably the increased visceral fat leads to increased intra-abdominal and intragastric pressure, resulting in a predisposition for hiatal hernia.
- Metabolic Syndrome: Metabolic syndrome is a risk factor for GERD and its progression. Subjects with hypercholesterolemia, hyperuricemia, enlarged waist circumference, hypertension, low HDL-cholesterol level, hypertriglyceridemia, and a diagnosis of metabolic syndrome were more likely to progress from a nonerosive esophagitis to erosive disease and less likely to regress from erosive to nonerosive states.
Symptoms of gastroesophageal reflux
People who experience heartburn at least two to three times a week may have gastroesophageal reflux disease, or GERD. The most common symptom of GERD, heartburn. Heartburn is experienced as a burning sensation in the center of the chest, which sometimes spreads to the throat; there also may be an acid taste in the throat. Less common symptoms include:
- Stomach pain (pain in the upper abdomen)
- Non-burning chest pain
- Difficulty swallowing (called dysphagia), or food getting stuck
- Painful swallowing (called odynophagia)
- Persistent laryngitis/hoarseness
- Persistent sore throat
- Chronic cough, new onset asthma, or asthma only at night
- Regurgitation of foods/fluids; taste of acid in the throat
- Sense of a lump in the throat
- Worsening dental disease
- Recurrent pneumonia
- Chronic sinusitis
- Waking up with a choking sensation
The following signs and symptoms may indicate a more serious problem, and should be reported to a healthcare provider immediately:
- Difficulty or pain with swallowing (feeling that food gets “stuck”)
- Unexplained weight loss
- Chest pain
- Choking
- Bleeding (vomiting blood or dark-colored stools)
Complications of gastroesophageal reflux
A number of serious complications can arise in patients with severe gastroesophageal reflux disease.
- Ulcers – Ulcers can form in the esophagus as a result of burning from stomach acid. In some cases, bleeding occurs. You may not be aware of bleeding, but it may be detected in a stool sample with a test called hemocult.
- Stricture – Damage from acid can cause the esophagus to scar and narrow, causing a blockage (stricture) that can cause food or pills to get stuck in the esophagus. The narrowing is caused by scar tissue that develops as a result of ulcers that repeatedly damage and then heal in the esophagus.
- Lung and throat problems – Some people reflux acid into the throat, causing inflammation of the vocal cords, a sore throat, or a hoarse voice. The acid can be inhaled into the lungs and cause a type of pneumonia (aspiration pneumonia) or asthma symptoms. Chronic acid reflux into the lungs may eventually cause permanent lung damage, called pulmonary fibrosis or bronchiectasis.
- Barrett’s esophagus – Barrett’s esophagus occurs when the normal cells that line the lower esophagus (squamous cells) are replaced by a different cell type (intestinal cells). This process usually results from repeated damage to the esophageal lining, and the most common cause is longstanding gastroesophageal reflux disease. The intestinal cells have a small risk of transforming into cancer cells.
- Esophageal cancer – There are two main types of esophageal cancer: adenocarcinoma and squamous cell carcinoma. A major risk factor for adenocarcinoma is Barrett’s esophagus, discussed above. Squamous cell carcinoma does not appear to be related to GERD.
Types of diagnosis and tests needed to evaluate GERD
Your doctor may decide to conduct one or more of the following tests.
Barium Esophagram or Upper GI X-Ray
This is a test where you are given a chalky material to drink while X-rays are taken to outline the anatomy of the digestive tract.
Endoscopy
This test involves insertion of a small lighted flexible tube through the mouth into the esophagus and stomach to examine for abnormalities. The test is usually performed with the aid of sedatives.
Esophageal Manometry
This test involves inserting a small flexible tube through the nose into the esophagus and stomach in order to measure pressures and function of the esophagus. With this test, the degree of acid refluxed into the esophagus can be measured as well.
24 Hours Esophageal pH study
A 24-hour esophageal pH study is the most direct way to measure the frequency of acid reflux. The test involves inserting a thin tube through the nose and into the esophagus. The tube is left in the esophagus for 24 hours. During this time the patient keeps a diary of symptoms. The tube is attached to a small device that measures how much stomach acid is reaching the esophagus.
Treatment and medications required for GERD
Lifestyle Changes
Medical treatment of GERD usually begins with dietary and life-style modifications. Common suggestions to help alleviate the symptoms of esophageal reflux:
- Avoid foods that increase gastric acidity.
- Avoid foods that decrease lower esophageal sphincter pressure.
- Avoid foods that affect peristalsis.
- Avoid foods that slow gastric emptying.
- Avoid large meals.
- Avoid smoking.
- Avoid lying down after meals.
- Elevate the head of the bed.
- Lose weight (if overweight).
- Avoid tight fitting clothing.
- Use Chew gum or use oral lozenges can increase saliva production, which may help to clear stomach acid.
Drug Therapy
- In some patients, simple implementation of these dietary and life-style changes is sufficient to control reflux symptoms.
- However, most patients who present to a physician with severe reflux symptoms or with esophagitis require drug therapy.
- Current drug therapy depends on two categories of drugs: those that decrease gastric acidity (acid-suppressing agents) and those that enhance upper gastrointestinal motility (prokinetic agents).
Antacids
- Antacids are commonly used for short-term relief of acid reflux. However, the stomach acid is only neutralized very briefly after each dose, so they are not very effective.
- Examples of antacids include Tums®, Maalox®, and Mylanta®.
Histamine antagonists
- The histamine antagonists reduce production of acid in the stomach. However, they are somewhat less effective than proton pump inhibitors.
- Examples of histamine antagonists available in the United States include ranitidine (Zantac®), famotidine (Pepcid®), cimetidine (Tagamet®), and nizatidine (Axid®).
- These medications are usually taken by mouth once or twice per day. Cimetidine, ranitidine, and famotidine are available in prescription and non-prescription strengths.
Proton Pump Inhibitors
- Proton Pump Inhibitors (PPIs) are drugs that block the final common pathway of acid secretion (Figure 12). P
- PIs block the effects of all three major pathways (histamine, acetylcholine, and gastrin) for acid stimulation.
- As a result, the acid suppressing capability of PPIs is substantially greater than that of H2 blockers.
- PPIs include omeprazole (Prilosec®), esomeprazole (Nexium®), lansoprazole (Prevacid®), dexlansoprazole (Kapidex®), pantoprazole (Protonix®), and rabeprazole (Aciphex®), which are stronger and more effective than the H2 antagonists.
Prokinetic Agents
- Prokinetic agents are drugs that enhance motor activity of the smooth muscle (characteristic of GI tract).
- Although potentially beneficial for improving the strength of esophageal peristalsis, the resting pressure of the LES, and the strength of gastric contractions, it appears that the most important influence of available prokinetic agents is on gastric motility.
- In standard doses, prokinetic agents are as effective as H2 blockers, but less effective than PPIs.
Surgical treatment.
- Prior to the development of the potent acid-reducing medications described above, surgery was used for severe cases of GERD that did not resolve with medical treatment.
- Because of the effectiveness of medical therapy, the role of surgery has become more complex. In general, anti-reflux surgery involves repairing the hiatus hernia and strengthening the lower esophageal sphincter.
- The most common surgical treatment is the laparoscopic Nissen fundoplication. This procedure involves wrapping the upper part of the stomach around the lower end of the esophagus.
- Although the outcome of surgery is usually good, complications can occur. Examples include persistent difficulty swallowing (occurring in about 5 percent of patients), a sense of bloating and gas (known as “gas-bloat syndrome”), breakdown of the repair (1 to 2 percent of patients per year), or diarrhea due to inadvertent injury to the nerves leading to the stomach and intestines
What can I do to prevent gastroesophageal reflux?
- Limit caffeine. Limit coffee to 2-3 cups per day. Limiting consumption of other caffeine-containing beverages (tea, soft drinks) may also be helpful.
- Avoid tight clothing. Tight belts, tight pants or girdles can increase the pressure on the stomach.
- Avoid foods that cause symptoms. Foods to avoid are:
- Spicy and fatty foods
- Tomato and citrus juices (such as grapefruit and orange juices)
- Chocolate, mints, coffee, tea, cola, and alcoholic drinks.
- Do not lie down after 2 hours of eating. Allow gravity to work. Also, avoid bending over at the waist to pick up things; instead bend at the knees.
- Stop smoking. If you cannot stop, decreasing the number of cigarettes you smoke may help.
- Bed blocks. Elevate the head of your bed 2-6 inches with wood blocks or bricks. Using extra pillows is NOT a good substitute. Use of a foam wedge beneath the upper half of the body is an alternative
- Maintain your ideal weight. Excess weight increases the amount of pressure constantly placed on your stomach. Even small amounts of weight loss may help.
- Eat smaller meals. Don’t overfill your stomach.
 Diseases Treatments Dictionary This is complete solution to read all diseases treatments Which covers Prevention, Causes, Symptoms, Medical Terms, Drugs, Prescription, Natural Remedies with cures and Treatments. Most of the common diseases were listed in names, split with categories.
Diseases Treatments Dictionary This is complete solution to read all diseases treatments Which covers Prevention, Causes, Symptoms, Medical Terms, Drugs, Prescription, Natural Remedies with cures and Treatments. Most of the common diseases were listed in names, split with categories.







this information is very helpful to me
After day sleep i feel difficulty in breathing and some food came back in my mouth
It might be due to acid reflux from the stomach. Please consult with gastroenterologist to know the problem elobratively.
is it possible there is pain in back and chest because of acid reflux
can asthmatic patient take antacid
Yes, offcourse can take antacid if the asthma patient suffers from GERD.
Waking up from bed with a Choking pain in the chest and food from the esophagus tends to flow into the air pipe causing a momentarily breathlessness. Common especially when I drink juice before going to bed
Reduce liquid items before going into the bed or before sleeping. For some people it may araise and come out of it.
I hate that I am suffering from this debilitating disease! I need help soooooo bad! I stay hungry and am always thirsty because of my difficulty in swallowing.
Please consult a doctor.
I have this problem for 6 months. now I’m OK. this is what I did.
step 1: small meals
step 2: take vitamin b complex 3 times a week.
step 3: avoid acidic foods
step 4: increase water intake.
step 5: eat 1 apple almost every meal.
Thanks for sharing your experience with us.
can ulcer cause waist pain and ear problem. can it affect memory
No, it doesn’t affect memory, instead it can spoil your digestive process.
my throat hurts, it bleeds small when I brush and clear my throat. pls help.
please consult a doctor to get rid of this problem.
A few days ago I slept in the night but in the morning,it was hard to me to Breath And I Notified a Doctor and they said,I should scan what inside it actually when I scan they said ,they didn’t found anything, and I don’t know what to do and the things worrying me Pls,can u help me.
Please do a master checkup for your health.
can alcer cause weaknesses in all your body muscles
I have a burning sensation in my troat and in my tongue..I had that before but now this burning sensation in my mouth I don’t know how to cure it.i have use some alternatives but after several hours it comes back again. what can I do.
please consult a doctor.
I have so much gas in my stomach and a burning sensation in my chest. please help.
please consult a doctor.
thanks for excellent explained
Thanks for excellent explanation
it’s been 5 yrs I taking omeprozole.if I stop them
I experience the
pains.i v done endoscopy and nothing was found.shud I take them forever?
Please consult a doctor.
is there relationship between GERD and IBS
Irritable bowel syndrome, or IBS, causes belly pain along with changes in bowel habits, either diarrhea or constipation. Gastroesophageal reflux disease, or GERD, causes acid reflux, commonly referred to as heartburn.
I have been dealing with bad bad acid reflux for over a year I’m tired in pain my Doctor don’t seem to care I’m at work with this I tried every thing over the counter I need real professional help and tell me what can I do because now I’m more depressed than ever because of this please tell me what can I do
For appropriate prescription please consult a doctor.
I really need help, I do feel pain in my throat and feel as if something get stock in my esophagus, I have taking series of medication prescribed by doctors, yet pains persist. Please what should I do?
Please follow the natural remedies.
how will one be sure he/she is no longer suffering from the disease?
If no symptoms of GERD is appearing.
please name the food that I will take to avoid recurring gerd
To avoid recurring GERD, consider a diet focused on non-citrus fruits (such as melons and apples), vegetables excluding acidic ones, lean proteins, whole grains, low-fat dairy, mild herbs and spices, and non-caffeinated beverages. Additionally, opt for healthy fats like olive oil and avoid fried and fatty foods. Keep a food diary to identify personal triggers, and consult with a healthcare professional or dietitian for personalized advice based on your specific condition.