Overview
Necrotizing enterocolitis (NEC) is an inflammation in the intestines (usually the colon) that can be life-threatening if not treated right away. NEC may affect only the lining of the intestine or its entire thickness. The damage caused by NEC to the intestinal tissues can cause a hole in the intestines that allows the bacteria normally present only in the intestinal tract to leak out into the abdomen and cause infection. Once this occurs, the infection can progress very quickly and is considered a medical emergency.
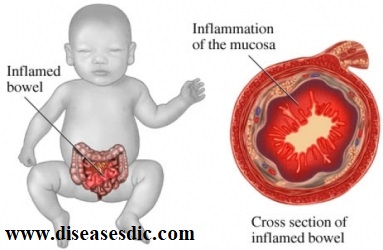
NEC most commonly affects premature babies, accounting for 60 to 80% of cases. It is the most common gastrointestinal emergency in the Neonatal Intensive Care Unit (NICU). It usually occurs within 3-12 days after birth.
Pathophysiology
It is not really understood what happens to cause necrotizing enterocolitis. The only risk factor identified is prematurity. As we mentioned earlier, when a baby is born premature, they are not born fully mature and developed. This may cause their gastrointestinal system to move slower than normal. If the intestines aren’t digesting food quickly enough, stool spends an increased time in the intestine and may contribute to bacterial growth. NEC also seems to develop when the baby is hypoxic, meaning their oxygen level in their blood is low, and they have hypoperfusion, meaning they are not getting enough oxygen to the cells within their body.
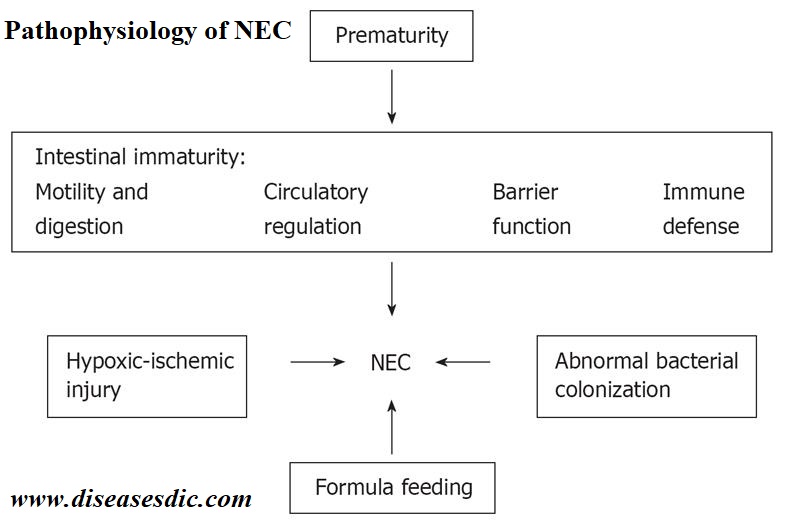
There are two factors which seem to be at play in NEC- enteral feedings and bacteria.
Enteral Feedings and NEC
Premature infants often receive enteral feedings, which consists of a tube that usually enters through their nose and travels into their stomachs. Since they are premature, they are unable to eat on their own, so formula is given through this tube to meet their nutritional requirements.
When a premature baby receives enteral feedings, it is believed to disrupt the integrity of the mucosa of the intestine. Their blood flow and the motility of their intestine are decreased. These factors cause the formula from their feedings to sit in the intestine unabsorbed and provides a perfect environment for bacteria to proliferate.
Receiving feedings in this manner when combined with bacteria proliferation injures the epithelial cells of the intestine. This causes inflammation, which can lead to necrotizing.
The Role of Bacteria in NEC
Before a baby is born, the intestine is a sterile environment. After they are born, bacteria will enter the intestines and ideally help to develop a normal intestinal immune system. Breastmilk helps in this development by helping to create a balanced flora of bacteria in the intestine. But in NEC, bacteria growth is rampant and is believed to be the toxic by-products induced by the food that is present in the intestines. Evidence does show that using breastmilk instead of formula helps to provide protection against the development of NEC.
What causes necrotizing enterocolitis (NEC)?
There is no single consistent cause of necrotizing enterocolitis. In most cases, a specific cause isn’t found. But experts believe these things might play a role:
- An underdeveloped (premature) intestine
- Too little oxygen or blood flow to the intestine at birth or later
- Injury to the intestinal lining
- Heavy growth of bacteria in the intestine that erodes the intestinal wall
- Viral or bacterial infection of the intestine
- Formula feeding (breastfed babies have a lower risk of NEC)
NEC sometimes seems to happen in “clusters,” affecting several infants in the same nursery. This might be coincidental, but some viruses and bacteria occasionally have been found in babies with NEC. NEC does not spread from one baby to another, but a virus or bacteria that cause it can. This is one reason all nurseries and NICUs have very strict precautions to help prevent the spread of infection.
Risk factors of NEC
Fortunately, NEC is rare. It can happen in any newborn baby, but it’s most common in premature babies who weigh less than 3.25 lbs. Others who may be at risk include:
- High-risk or premature babies who are fed formula by mouth or tube
- Those who had a difficult delivery or have lowered oxygen levels
- Infants who have too many red blood cells in circulation
- Babies with existing gastrointestinal infections
- Seriously ill infants and those who’ve received a blood transfusion
What are the symptoms of NEC?
The symptoms of NEC often include the following:
- Swelling or bloating of the abdomen
- Discoloration of the abdomen
- Bloody stool
- Diarrhea
- Poor feeding
- Vomiting

Your baby may also show symptoms of an infection, such as:
- Apnea, or disrupted breathing
- A fever
- Lethargy
Complications of necrotizing enterocolitis
Damage to the intestinal tissues can lead to perforation (a hole) in the intestines. This allows the bacteria normally present in the intestinal tract to leak out into the abdomen and cause infection. The damage may only exist in a small area or it may progress to large areas of the intestine. The disease can progress very quickly. Infection in the intestines can be overwhelming to a baby and, even with treatment, there may be serious complications. Problems from NEC may include the following:
- Perforation (hole) in the intestine
- Scarring or strictures (narrowing) of the intestine
- Problems with food absorption if large amounts of intestine must be removed
- Severe, overwhelming infection
Diagnosis and Test to detect NEC
A thorough physical examination of the baby along with symptoms is carried out. The following investigations are also done:
- X-ray of the baby’s belly.
- Fecal occult blood test is done to check for blood in the baby’s stool.
- Tests are done to look for bacteria in the blood, stool, urine or spinal fluid.

NEC diagnosis can be categorized into three stages depending on the extent of the infection and the symptoms displayed (5).
- Stage 1 – Suspected NEC: The baby would display non-specific or general symptoms that could indicate necrotizing enterocolitis. Symptoms include lethargy, fussiness, and fever. An X-ray in this stage displays abdominal distention or gastric residues but not the extent to prove it to be NEC.
- Stage 2 – Proven NEC: X-rays show clear signs of NEC with the presence of large gas globules within the intestine. Bowel sounds will be absent due to a dysfunctional intestine.
- Stage 3 – Advanced NEC: The intestine is damaged to the extent that there are holes in the intestinal wall. The baby also has severe sleep apnea, low blood pressure, and inflammation of the entire abdominal wall.
Treatment and Medications
- Treatment for Necrotizing Enterocolitis depends on the severity of the condition, the age of the baby and the general health of the baby.
- Necrotizing enterocolitis treatment can last for a week to 10 days.
- The baby will be admitted to the hospital’s neonatal intensive care unit (NICU).
- The baby suffering from Necrotizing enterocolitis is fed intravenously. All oral feedings are stopped.
- Antibiotics are given to fight with the infection associated with Necrotizing enterocolitis.
- A tube is inserted through the nose to the stomach which removes excess fluids and gas present in the intestine.
- Surgery for Necrotizing enterocolitis is done in severe cases where the baby is not getting better or if perforation develops in the intestine.
- Around 1 out of 4 babies having necrotizing enterocolitis need surgery.
- Surgery for Necrotizing Enterocolitis is done in two parts with these two procedures being weeks or months apart.
- The first surgery for Necrotizing enterocolitis involves removing the damaged/dead parts of the intestine and creating an ileostomy or a colostomy. This is done so that the intestine can rest and heal.
- In ostomy, the stool exits the body via an opening in the belly and gets collected in a bag.
- The second surgical treatment for Necrotizing enterocolitis is done to close the ostomy site and allow the stool to pass normally through the body again.
- After the treatment for Necrotizing enterocolitis is complete, the baby will be discharged if he/she is accepting feeds and not losing weight.
- The nurse from the hospital will instruct you on how to feed and care for the baby at home.
- Parents of the baby tend to feel overwhelmed regarding the baby’s health. It is advised to consult with a counselor or a social worker regarding your feelings and to relieve stress.
How to Prevent Necrotizing Enterocolitis?
There is no precise prevention for necrotizing enterocolitis since its cause is not apparent. However, you can take precautions after consulting with the doctor if your baby falls into the high-risk category. Here is what you can do to reduce the risk of NEC in your baby:
- Breast milk: Pediatric experts note that babies who have only breast milk are not so much at risk of NEC Premature babies who are given food through tubes (enteral feeding) should be given expressed milk to minimize NEC risk. Breast milk is also beneficial for low birth weight infants. A study has found that providing low birth-weight babies a feed consisting of at least 50% breast milk in the first 14 days after birth reduces the risk of NEC by six times (6).
- Delaying feed: Feeding through the mouth can be delayed in the case of premature babies whose gastrointestinal tract is still underdeveloped and immature. You can consider it after doctor’s consultation. In any case, your infant would be in intensive care at the hospital, which might delay oral feeding anyway.
- Probiotics: Probiotic bacteria such as Bifidus infantis and Lactobacillus acidophilus can help reduce the risk. But there is limited research on their efficacy, the precise dosage, and the type of bacteria that works. Consult your doctor before adopting this measure.
 Diseases Treatments Dictionary This is complete solution to read all diseases treatments Which covers Prevention, Causes, Symptoms, Medical Terms, Drugs, Prescription, Natural Remedies with cures and Treatments. Most of the common diseases were listed in names, split with categories.
Diseases Treatments Dictionary This is complete solution to read all diseases treatments Which covers Prevention, Causes, Symptoms, Medical Terms, Drugs, Prescription, Natural Remedies with cures and Treatments. Most of the common diseases were listed in names, split with categories.






which type of medicine will be given to surch patient
Various antibiotic regimens can be employed; one frequently used regimen includes ampicillin, aminoglycoside (eg, gentamicin) or third-generation cephalosporin (cefotaxime), and clindamycin or metronidazole.