Overview
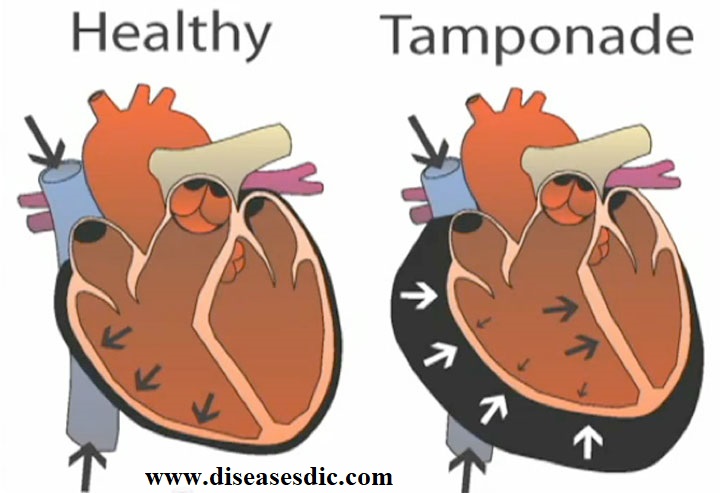
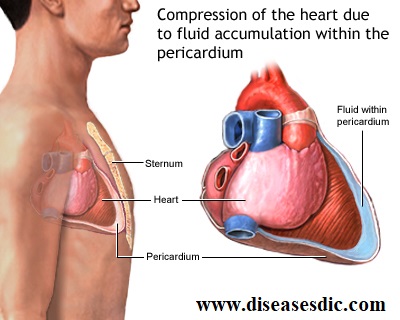
Cardiac tamponade is a serious medical condition in which blood or fluids fill the space between the sac that encases the heart and the heart muscle. This places extreme pressure on your heart. The pressure prevents the heart’s ventricles from expanding fully and keeps your heart from functioning properly. Your heart can’t pump enough blood to the rest of your body when this happens. This can lead to organ failure, shock, and even death.
Pathophysiology
Cardiac tamponade occurs when increased pressure within the pericardial sac, caused by the excess fluid, becomes sufficient to restrict the filling of the heart during diastole. Since the heart can no longer fill completely, less blood is ejected with each heartbeat, and the heart has to work much harder to supply the body’s needs. Furthermore, the blood trying to enter the heart tends to back up, producing congestion in the lungs and veins.
The amount of pericardial fluid which is necessary to produce tamponade depends on to a great extent on how rapidly the fluid has accumulated. If pericardial fluid increases rapidly, the pericardium does not have time to “stretch,” and the pressure within the pericardial space can increase greatly— even with a relatively small amount of fluid. On the other hand, if the pericardial fluid accumulates more gradually (say, over a period of days or weeks), the pericardium has time to stretch out to accommodate the extra fluid. In this case, the pressure within the pericardial space may not increase substantially until the pericardial effusion has become quite large, to the point at which the pericardium is incapable of stretching any further.
Phases of Cardiac Tamponade
3 phases of hemodynamic changes in tamponade, as follows:
- Phase I – The accumulation of pericardial fluid impairs relaxation and filling of the ventricles, requiring a higher filling pressure; during this phase, the left and right ventricular filling pressures are higher than the intrapericardial pressure
- Phase II – With further fluid accumulation, the pericardial pressure increases above the ventricular filling pressure, resulting in reduced cardiac output (see the Cardiac Output calculator)
- Phase III – A further decrease in cardiac output occurs, which is due to the equilibration of pericardial and left ventricular (LV) filling pressures
Causes
Cardiac tamponade is usually the result of penetration of the pericardium, which is the thin, double-walled sac that surrounds your heart. The cavity around your heart can fill with enough blood or other bodily fluids to compress your heart. As the fluid presses on your heart, less and less blood can enter. Less oxygen-rich blood is pumped to the rest of your body as a result. The lack of blood getting to the heart and the rest of your body can eventually cause shock, organ failure, and cardiac arrest.
The causes of pericardial penetration or fluid accumulation might include:
- Gunshot or stab wounds
- Blunt trauma to the chest from a car or industrial accident
- Accidental perforation after cardiac catheterization, angiography, or insertion of a pacemaker
- Punctures made during placement of a central line, which is a type of catheter that administers fluids or medications
- Cancer that has spread to the pericardial sac, such as breast or lung cancer
- A ruptured aortic aneurysm
- Pericarditis, an inflammation of the pericardium
- Lupus, an inflammatory disease in which the immune system mistakenly attacks healthy tissues
- High levels of radiation to the chest
- Hypothyroidism, which increases the risk for heart disease
- A heart attack
- Kidney failure
- Infections that affect the heart
Risk factors of Cardiac Tamponade
Some of the known risk factors for Cardiac Tamponade are:
- End-stage renal disease (causing complete failure of kidney function)
- Undergoing invasive procedures on the heart and lung
- Exposure to infections (such as tuberculosis): Sometimes, healthcare personnel may come in contact with infected individuals; or those living in regions where tuberculosis is prevalent, e.g., Asia and Mexico
- The period following an episode of heart attack
- Individuals with collagen vascular disorders such as lupus and rheumatoid arthritis
- Individuals with certain tumors, such as end-stage lung tumors
Cardiac Tamponade associated with trauma or HIV is more common in young adults, whereas tamponade due to malignancy and/or renal failure occurs more frequently in the elderly.
It is important to note that having a risk factor does not mean that one will get the condition. A risk factor increases ones chances of getting a condition compared to an individual without the risk factors. Some risk factors are more important than others.
Also, not having a risk factor does not mean that an individual will not get the condition. It is always important to discuss the effect of risk factors with your healthcare provider.
Symptoms of Cardiac Tamponade
Signs and Symptoms of Cardiac Tamponade may include:
- Anxiety, restlessness
- Sharp chest pain that is felt in the neck, shoulder, back, or abdomen
- Chest pain that gets worse with deep breathing or coughing
- Problems breathing
- Discomfort, sometimes relieved by sitting upright or leaning forward
- Fainting, lightheadedness
- Pale, gray, or blue skin
- Palpitations
- Rapid breathing
- Swelling of the legs or abdomen
- Jaundice
Other symptoms that may occur with this disorder:
- Dizziness
- Drowsiness
- Weak or absent pulse
Complications
The course of Cardiac Tamponade varies, being dependent upon the underlying cause and speed of onset. The complications may include:
Even if there is a slow development of Cardiac Tamponade over a period of time, it can cause permanent damage to the heart. When not treated early, this can affect the pumping efficiency of the heart and also lead to pulmonary edema (fluid accumulation in the lungs)
When sudden, Cardiac Tamponade can be fatal without treatment. In such a case, if early treatment is not provided, it can interfere with the pumping capacity of heart, eventually causing a heart failure leading to death
Diagnosis and test
These tests may be helpful in helping determine the presence and cause of cardiac tamponade.
Lab Studies:
- Full blood picture – blood is taken to measure the level of haemoglobin, red cells, white cells, etc.
- Creatine kinase and isoenzymes – Enzymes released when heart muscle is damaged, such as CK-MB, Troponin T/I, may be elevated.
- ECG – provides an electrical picture of the heart and can demonstrate low voltages and/or alternating sizes of complexes.
Imaging Studies:
- Chest x-ray: The heart may appear large, globular or pear shaped with sharp outlines. In cardiac tamponade, the chest x-ray may demonstrate an enlarged heart shape after 200-250 mL of slow fluid accumulation. A normal cardiac picture seen in patients with rapid accumulation of fluid or blood.
- Echocardiography: Most useful technique for demonstrating fluid in the pericardial sac and can show collapse of the right pumping chamber of the heart (ventricle) when the heart relaxes.
- Doppler: May show increased flow through specific valves in the heart.
- Magnetic Resonance Imaging: May detect blood or fluid around the heart.
Treatment and medications
As cardiac tamponade can result in shock or death, it always requires emergency medical treatment. This treatment involves draining excess fluid from around the heart.
A doctor may use the following methods to remove the fluid and reduce the pressure on the heart:
- Pericardiocentesis. The removal of fluid from the pericardium using a needle.
- Pericardiectomy. The surgical removal of part of the pericardium to relieve pressure on the heart.
- Thoracotomy. A surgical procedure that allows the draining of blood or blood clots around the heart.
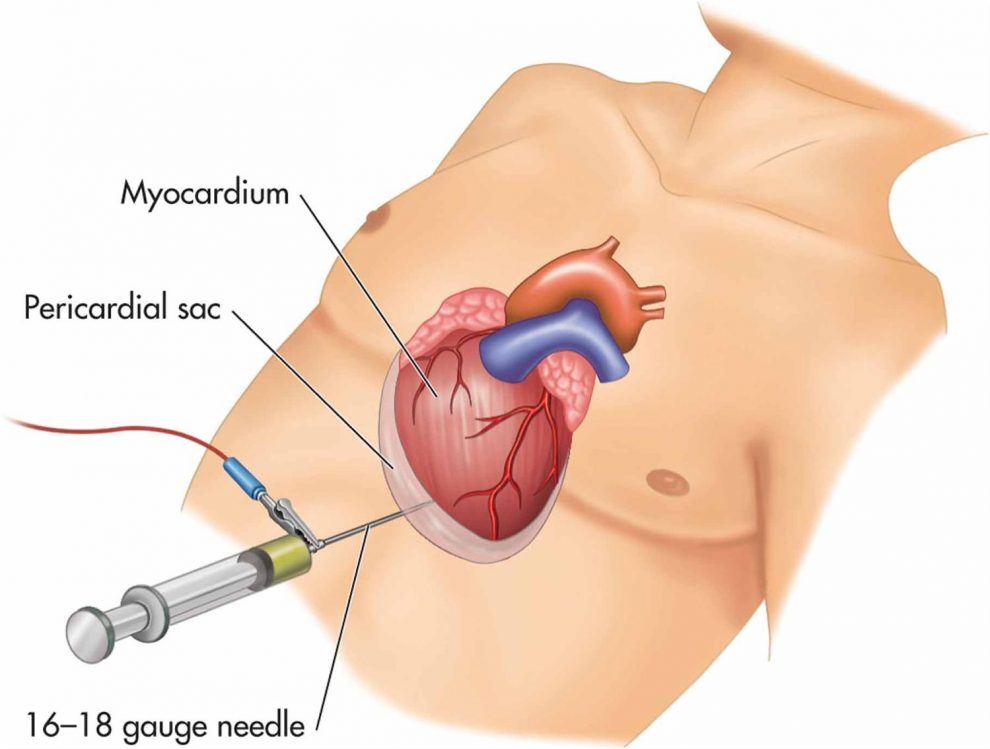
According to some research, doctors should choose minimally invasive procedures, such as pericardiocentesis, as the first treatment option. Such options carry a less significant risk of complications and have lower mortality rates.
However, more complicated cases of cardiac tamponade will often require surgery, including a thoracotomy.
After surgery, the individual may receive the following as they stabilize:
- Intravenous (IV) fluids to maintain normal blood pressure
- Medications to increase blood pressure
- Oxygen to reduce stress on the heart
Once the person is stable, the doctor will need to determine and treat the underlying cause of the cardiac tamponade to prevent further complications.
Prevention
You can cut your risk for some of the health problems that can lead to cardiac tamponade. For example, take care of your heart by:
- Eating a heart-healthy diet
- Getting enough exercise
- Maintaining a healthy weight
- Avoiding too much alcohol
- Seeing a healthcare provider regularly to treat any health problems
Many cases of cardiac tamponade cannot be prevented, though.
 Diseases Treatments Dictionary This is complete solution to read all diseases treatments Which covers Prevention, Causes, Symptoms, Medical Terms, Drugs, Prescription, Natural Remedies with cures and Treatments. Most of the common diseases were listed in names, split with categories.
Diseases Treatments Dictionary This is complete solution to read all diseases treatments Which covers Prevention, Causes, Symptoms, Medical Terms, Drugs, Prescription, Natural Remedies with cures and Treatments. Most of the common diseases were listed in names, split with categories.








Great and having sharp pains in my chest get to my back, pains on my ribs.Sometimes, l feel cold and sweating at the same time and also body itches.Consultation says l have but gastritis. l drink alcohol also.Kindly advice.
Please consult a doctor.
what are the possible drugs to be used to reduce the fluids around the chest region without the surgery or extraction with needles
The role of medication therapy in cardiac tamponade is limited.
can it be treated with helbs
No, it can’t be treated with herbs but it is possible only with surgery or medications.
csuse of heart attack
There are many causes, to know more please look into the post.
very nice and important information.
iam struggle with this condition and i dont have money to get help must i die and iam 55years old
Please contact a charitable trust nearby your locality to avail support for your treatment.
Thanks a lot detail study and advoice to enough precautions
I was treated for cardiac Temponade on 8th February 2018,after AVR surgery on 29 th January,now I am well,but my BP remains fluctuating,sometimes it raises to 180/100,after rest,it comes normal,I am also taking 38.5 ug Thyronorm,TSH is 6.79,tested yesterday.HR remains 50 to 65pm,I am 64 years to complete on 14 th August 2019.
what is the difference between cardiac tamponade and pericardial effusion?
Pericardial effusion involves the gradual accumulation of fluid around the heart’s pericardial sac, causing symptoms like chest pain and shortness of breath. Cardiac tamponade is a more critical condition, characterized by rapid fluid buildup, leading to life-threatening symptoms such as low blood pressure and impaired cardiac function.