Definition
Pneumonia is an infection in one or both lungs. It can be caused by bacteria, viruses, or fungi. Bacterial pneumonia is the most common type in adults. Pneumonia causes inflammation in the air sacs in your lungs, which are called alveoli. The alveoli fill with fluid or pus, making it difficult to breathe.
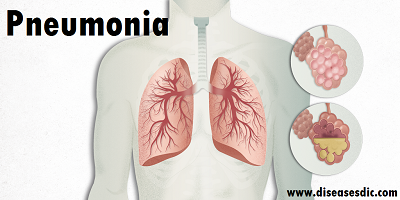
Normal air sacs and pneumonia affected air sacs
History
Pneumonia has been a common disease throughout human history. The word is from Greek πνεύμων (pneúmōn) meaning “lung”. The symptoms were described by Hippocrates (c. 460 BC – 370 BC). Edwin Klebs was the first to observe bacteria in the airways of persons having died of pneumonia in 1875.
Initial work identifying the two common bacterial causes, Streptococcus pneumoniae and Klebsiella pneumoniae, was performed by Carl Friedländer and Albert Fraenkel in 1882 and 1884, respectively.
Friedländer’s initial work introduced the Gram stain, a fundamental laboratory test still used today to identify and categorize bacteria. Christian Gram’s paper describing the procedure in 1884 helped to differentiate the two bacteria, and showed that pneumonia could be caused by more than one microorganism
Epidemiology
One study estimated that nearly 4 million children died each year of acute respiratory infections in the period from 1980 to 1990. Because of this, the World Health Organization (WHO) set up the Child Health Epidemiology Reference Group (CHERG) to further study the incidence of childhood pneumonia.
CHERG performed systematic reviews to compile pneumonia statistics in children under age 5 for the year 2000. The group found that there were approximately 150 million new episodes of pneumonia in children under 5. Of these 150 million new cases, approximately 4 million occurred in developed countries, while the rest occurred in developing nations.
Pneumonia types
Types by location
Community-acquired pneumonia (CAP) as the name implies, develops outside of the hospital or health-care environment. It is more common than hospital-acquired pneumonia. CAP is most common in winter and affects about 4 million people a year in the U.S.
Hospital-acquired pneumonia (HAP) is acquired when an individual is already hospitalized for another condition. HAP is generally more serious because it develops in ill patients already hospitalized or under medical care for another condition. Being on a ventilator for respiratory support increases the risk of acquiring HAP. Health-care-associated pneumonia is acquired from other health-care settings, like kidney dialysis centers, outpatient clinics, or nursing homes.
Types by germ
Pneumonia can be classified according to the organism that caused the infection.
Bacterial pneumonia: The most common cause of bacterial pneumonia is Streptococcus pneumoniae. Chlamydophila pneumonia and Legionella pneumophila can also cause bacterial pneumonia.
Viral pneumonia: Respiratory viruses are often the cause of pneumonia, especially in young children and older people. Viral pneumonia is usually not serious and lasts for a shorter time than bacterial pneumonia.
Mycoplasma pneumonia: Mycoplasma organisms are not viruses or bacteria, but they have traits common to both. Mycoplasmas generally cause mild cases of pneumonia, most often in older children and young adults.
Fungal pneumonia: Fungi from soil or bird droppings can cause pneumonia in people who inhale large amounts of the organisms. They can also cause pneumonia in people with chronic diseases or weakened immune systems.
Pneumonia Risk factors
Those most at risk include people who:
- Are aged under 5 years or over 65years
- Smoke tobacco, consume large amounts of alcohol, or both have underlying conditions such as cystic fibrosis, chronic obstructive pulmonary disorder (COPD), asthma, or conditions that affect the kidneys, heart, or liver
- Have a weakened or impaired immune system, due, for example, to AIDS, HIV, or cancer
- Take medicines forgastroesophageal reflux disease (GERD)
- Have recently recovered from a cold or influenza infection
- Experience malnutrition
- Have been recently hospitalized in an intensive care unit
- Have been exposed to certain chemicals or pollutants
Some groups are more prone than others to pneumonia, including Native Alaskan or certain Native American ethnicities.
Causes of Pneumonia
- Bacteria and viruses are the main causes of pneumonia. Pneumonia-causing germs can settle in the alveoli and multiply after a person breathes them in.
- Pneumonia can be contagious. The bacteria and viruses that cause pneumonia are usually inhaled.
- They can be passed on through coughing and sneezing, or spread onto shared objects through touch.
- The body sends white blood cells to attack the infection. This is why the air sacs become inflamed. The bacteria and viruses fill the lung sacs with fluid and pus, causing pneumonia.
Symptoms
Pneumonia symptoms can be mild to life-threatening. The most common symptoms of pneumonia can include:
- coughing that may produce phlegm (mucus)
- fever, sweating, and chills
- shortness of breath
- chest pain
Other symptoms can vary according to the cause and severity of the infection, as well as the age and general health of the individual.
Symptoms by cause
- Viral pneumoniamay start with flu-like symptoms, such as wheezing. A high fever may occur after 12–36 hours.
- Bacterial pneumoniamay cause a fever as high as 105°F along with profuse sweating, bluish lips and nails, and confusion.
Symptoms by age
- Children under 5 years of age may have fast breathing.
- Infants may vomit, lack energy, or have trouble drinking or eating.
- Older people may have a lower-than-normal body temperature.
Diagnosis and test
Typically, it can be diagnosed with the physical exam and the chest X-ray. But depending on the severity of your symptoms and your risk of complications, your doctor may also order one or more of these tests:
A blood test: This test can confirm an infection, but it may not be able to identify what’s causing it.
A sputum test: This test can provide a sample from your lungs that may identify the cause of the infection.
Pulse oximetry: An oxygen sensor placed on one of your fingers can indicate whether your lungs are moving enough oxygen through your bloodstream.
A urine test: This test can identify the bacteria Streptococcus pneumoniae and Legionella pneumophila.
A CT scan: This test provides a clearer and more detailed picture of your lungs.
A fluid sample: If your doctor suspects there is fluid in the pleural space of your chest, they may take fluid using a needle placed between your ribs. This test can help identify the cause of your infection.
A bronchoscopy: This test looks into the airways in your lungs. It does this using a camera on the end of a flexible tube that’s gently guided down your throat and into your lungs. Your doctor may do this test if your initial symptoms are severe, or if you’re hospitalized and your body is not responding well to antibiotics.
Treatment and medications
Your treatment will depend on the type of pneumonia you have, how severe it is, and your general health.
Prescribed treatment
- Antibiotic, antiviral, and antifungal drugs are used to treat pneumonia, depending on the specific cause of the condition. Most cases of bacterial pneumonia can be treated at home with oral antibiotics, and most people respond to the antibiotics in one to three days.
- Your doctor may also recommend over-the-counter (OTC) medication to relieve your pain and fever, as needed. These may include aspirin, ibuprofen(Advil, Motrin), and acetaminophen (Tylenol).
- Your doctor may also recommend cough medicine to calm your cough so you can rest. However, coughing helps remove fluid from your lungs, so you don’t want to eliminate it entirely.
Home treatment
You can help your recovery and prevent a recurrence by:
- Taking your drugs as prescribed
- Getting a lot of rest
- Drinking plenty of fluids
- Not overdoing it by going back to school or work too soon
Hospitalization
If your symptoms are very severe or you have other health problems, you may need to be hospitalized. At the hospital, doctors can keep track of your heart rate, temperature, and breathing. Treatment may include:
- Intravenous antibiotics: These are injected into your vein.
- Respiratory therapy: This therapy uses a variety of techniques, including delivering specific medications directly into the lungs. The respiratory therapist may also teach you or help you to perform breathing exercises to maximize your oxygenation.
- Oxygen therapy: This treatment helps maintain the oxygen level in your bloodstream. You may receive oxygen through a nasal tube or a face mask. If your case is extreme, you may need a ventilator (a machine that supports breathing).
Dietary management for Pneumonia
- Drink plenty of fluids and fresh juice of fruits and vegetables.
- Consume hot vegetable soups – tomato, sweet corn, etc.
- Add a pinch of turmeric to your diet as it has anti-inflammatory properties.
- Initially, the diet should consist of fresh fruits and vegetables when better can start with grains and little of protein in diet.
- Milk and milk products and sweets should be avoided to decrease mucus production.
- Onion and garlic should be consumed it is beneficial.
- Boil a mixture of Bishops weed (Ajwain), tea leaves and water and inhale the steam, helps to decongest. Do this at least 2-3 times a day.
- Gargle with warm water, a pinch of salt and turmeric to soothe your throat.
- Consume lots of vitamin A, maintains the integrity of the respiratory mucosa: Liver oils of fish like cod, shark, and halibut are richest source of vitamin A.
- Increase intake of vitamin C, it has the antioxidant property: foods of animal origin are poor in vitamin C.
- Include zinc in your diet, it boosts up your immunity:
Prevention of Pneumonia
Experts recommend immunization for children and adults. Children get the pneumococcal vaccine as part of their routine shots. Two different types of pneumococcal vaccines are recommended for people ages 65 and older. If you smoke, or you have a long-term health problem, it’s a good idea to get a pneumococcal vaccine. It may not keep you from getting pneumonia. But if you do get pneumonia, you probably won’t be as sick. You can also get an influenza vaccine to prevent the flu because sometimes people get pneumonia after having the flu.
You can also lower your chances of getting pneumonia by staying away from people who have a cold, measles, or chickenpox and iou may get pneumonia after you have one of these illnesses. Wash your hands often. This helps prevent the spread of viruses and bacteria that may cause pneumonia.