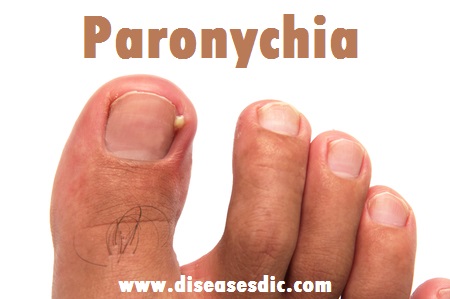
Definition
Paronychia is an infection of the skin around a fingernail or toenail. The infected area can become swollen, red, and painful, and a pus-filled blister (abscess) may form. Most of the time, paronychia is not serious and can be treated at home. In rare cases, the infection can spread to the rest of the finger or toe and lead to a deeper infection that may require a doctor’s help. It’s unlikely that your child will get paronychia in a toe (unless he or she has an ingrown toenail). But fingernail paronychia is one of the most common hand infections.
Nail Structure and Function
The nail is a complex unit composed of five major modified cutaneous structures: the nail matrix, nail plate, nail bed, cuticle (eponychium), and nail folds. The cuticle is an outgrowth of the proximal fold and is situated between the skin of the digit and the nail plate, fusing these structures together. This configuration provides a waterproof seal from external irritants, allergens, and pathogens.
Types of Paronychia
There are primarily two types of paronychia which may develop around the finger or toenails. These are classified by the time duration that the skin infection lasts.
Acute Paronychia: The skin infection develops fast and lasts for a few days in acute paronychia. This kind of paronychia is seen following skin breaks during a manicure, or when infection sets into an ingrown toenail. It is usually bacterial in nature, often caused by straphylococcus aureus bacteria. However, germs from the cold sore virus like herpes simplex or yeast such as Candida may also cause the condition.
Chronic Paronychia: The infection develops slowly and may last for many weeks. In such cases, a mix of multiple pathogens causes the infection. A combination of yeast like candida, virus like herpes simplex, and bacteria like Staphylococcus aureus may be found. This condition is commonly found in people who have to work with their hands constantly being exposed to water, chemicals and detergents. It has a tendency to reoccur even after being treated and cured.
The third variety of paronychia is a subungual abscess, which occurs in the same location as a subungual hematoma and presents with pain and entrapped pus that is visible between the nail plate and the nail bed
Risk factors of Paronychia
- Acute: direct or indirect trauma to cuticle or nail fold, manicured/sculptured nails, nail biting, thumb sucking, manipulating a hangnail
- Chronic: frequent immersion of hands in water with excoriation of the lateral nail fold (e.g., chefs, bartenders, housekeepers, swimmers, dishwashers, nurses)
- Predisposing conditions such as diabetes mellitus (DM) and immunosuppression
- Medications such as EGFR inhibitors, systemic retinoids, chemotherapy and antiretroviral agents
Causes of Paronychia
The infection occurs when the skin around the nail becomes damaged, allowing germs to enter.
Bacteria or fungi can cause paronychia, and common culprits are Staphylococcus aureus and Streptococcus pyogenes bacteria.
Common causes of skin damage around the nail include:
- Biting or chewing the nails
- Clipping the nails too short
- Manicures
- Excessive exposure of the hands to moisture, including frequently sucking the finger
- Ingrown nails
Paronychia Symptoms
If your child has paronychia, it’s usually easy to recognize. Look for:
- An area of red, swollen skin around a nail that’s painful, warm, and tender to the touch
- A pus-filled blister
A pus-filled blister
Bacterial paronychia:
- Usually appears very suddenly
Fungal paronychia:
- Can take longer to notice and causes less obvious symptoms
- Can be a chronic condition (last for a long time)
Chronic paronychia can cause changes in the affected nail. It might turn a different color or look as though it is detached or abnormally shaped.
In rare cases, if the paronychia is especially severe and goes untreated, the infection can spread beyond the area of the nail.
Complications
Systemic implications and complications are rare but may include:
- Abscess formation
- Permanent deformation of the nail plate
- Systemic fever/chills
- Development of red streaks along the skin
- Development of cellulitis or erysipelas
- Joint pain
- General ill feeling
- Flu-like symptoms
- Osteomyelitis
- Flexor tenosynovitis
Diagnosis and test
Paronychia is a clinical diagnosis, often supported by laboratory evidence of infection.
- Gram stain microscopy may reveal bacteria
- Potassium hydroxide microscopy may reveal fungi
- Bacterial culture
- Viral swabs
- Tzanck smears
- Nail clippings for culture (mycology).
Treatment and medications
- Paronychia is typically treated with antibiotics, although milder acute cases can often resolve on their own without treatment. The antibiotics most commonly used to treat paronychia are Bactrim (TMP/SMX) and a cephalosporin named Keflex (cephalexin).
- If an anaerobic bacterium is suspected, Evoclin (clindamycin) or Augmentin (amoxicillin-clavulanate) may be given with Bactrim. Bactrim is especially effective against drug-resistant bacteria, including methicillin-resistant Staphylococcus aureus.
- In severe cases, a physician can elevate the hardened bit of skin bordering the nail itself (eponychium) so that pus can be drained. Alternatively, the doctor can directly slice into the fluctuant portion of the infection; this procedure is no different from draining an abscess or boil.
- Because paronychia are pretty superficial, anesthesia is unnecessary to drain most infections of pus. In fact, anesthetizing the area will likely result in added pain with little benefit.
- Sometimes paronychia can extend under part of the nail. In these cases, either part or all the nail needs to be removed. A paronychia that is left untreated can sometimes surround the entire nail margin and result in a “floating” nail.
- After a paronychia is drained of pus, there is usually no need for antibiotics. However, if the paronychia is accompanied by localized cellulitis or skin infection, then antibiotics are needed to treat the skin infection.
Surgical treatment of acute paronychia
Paronychia home care
Follow these guidelines when caring for yourself at home:
Clean and soak the toe or finger. Do this 2 times a day for the first 3 days. To do so:
- Soak your foot or hand in a tub of warm water for 5 minutes. Or hold your toe or finger under a faucet of warm running water for 5 minutes.
- Clean any crust away with soap and water using a cotton swab.
- Put antibiotic ointment on the infected area.
Change the dressing daily or any time it gets dirty.
If you were given antibiotics, take them as directed until they are all gone.
If your infection is on a toe, wear comfortable shoes with a lot of toe room. You can also wear open-toed sandals while your toe heals.
You may use over-the-counter medicine (acetaminophen or ibuprofen) to help with pain, unless another medicine was prescribed. If you have chronic liver or kidney disease, talk with your healthcare provider before using these medicines. Also talk with your provider if you’ve had a stomach ulcer or gastrointestinal bleeding.
Prevention
To help reduce your chances of paronychia:
- Keep your hands and feet clean and dry. Use a moisturizer after hand washing.
- Wear rubber gloves if you often come in contact with water or chemicals.
- Avoid biting or picking your nails.
- Practice proper hygiene. Do not share bathroom supplies.
- Avoid cutting, pulling, or tearing your cuticles.
- Avoid artificial nails, vigorous manicures, or treatments that remove the cuticles.