Definition
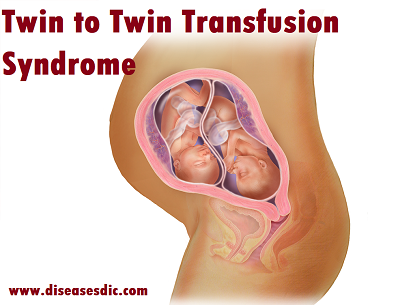
Twin to twin transfusion syndrome (TTTS) is a serious condition that occurs in approximately 10 to 15 percent of pregnancies with identical twins that share one placenta, also called a monochorionic-diamniotic twin pregnancy. Blood vessel connections within the placenta allow the fetuses to share blood supply and can cause an imbalance in the fetal blood volumes. As a result of unequal blood flow, one twin (the donor twin) pumps blood to the other twin (recipient twin). The condition can cause the recipient twin to make too much urine, which may enlarge the bladder, produce too much amniotic fluid, and in advanced stages, cause heart failure. The donor twin will then have decreased blood volume, low levels of amniotic fluid and urine, and a smaller bladder.
The stages of twin-to-twin transfusion syndrome
Twin-to-twin transfusion syndrome is organized into five stages:
Stage I: There is an imbalance in amniotic fluid between the twins.
Stage II: The bladder of the donor twin is “absent,” meaning it does not fill with urine and is not visible on an ultrasound exam.
Stage III: The excessive blood flow starts to cause problems with the recipient twin’s circulation. This can be detected through abnormalities in blood-flow patterns, which can be seen on an ultrasound.
Stage IV: The heart of the recipient twin begins to fail because of excessive fluid retention. This can be seen as fluid collections around the abdomen and the chest.
Stage V: One or both twins die from severe TTTS.
For stage I, the pregnancy will be monitored closely. “It can stop progressing beyond stage I
Causes
The placenta is a very active organ and provides babies with oxygen and nutrients during pregnancy. It grows along with the babies. Sometimes, for reasons that are not well understood, the normal flow of blood in the placenta’s blood vessels develops an abnormal pattern. When unborn babies share a placenta, the result can be an imbalance in blood circulation, with one baby receiving too much blood through the umbilical cord and the other receiving too little. It is this imbalance that leads to TTTS.
Risk factors
Being pregnant with identical twins or multiples puts a woman at risk for having a pregnancy complicated by TTTS. However, TTTS is an indiscriminate condition, occurring at random in monochorionic pregnancies.
Symptoms of twin to twin transfusion syndrome
Mothers may experience the following symptoms, all of which are due to the excess amniotic fluid around the recipient twin:
- Breathlessness
- Tightness in the abdomen or unusually rapid expansion of abdomen
- Rapid weight gain
- Pressure on the stomach
- Premature contractions
Normal monochorionic diamniotic (identical) twins with a shared placenta and connecting blood vessels
Identical twins with twin-to-twin transfusion syndrome (TTTS)
Complications of twin to twin transfusion syndrome
The complications that may occur when your twins have TTTS include:
- Selective intrauterine growth restriction (sIUGR): A more complicated state of TTTS where one baby may only have a small amount of the placenta
- Cardiomyopathy
- Premature labor
- A condition called twin anemia-polycythemia sequence (TAPS), where one fetus has a low blood count and the other has high blood count
- Loss of one or both fetuses
Complications in the recipient twin
With TTTS, the recipient twin is receiving more fluid and their heart is pumping against higher blood pressure. As a result, they are producing too much urine, which causes a significant increase in amniotic fluid. Other potential problems can occur in the recipient twin, including:
- Heart failure
- Demise or loss of the twin
Complications in the donor twin
Lacking fluid and blood, the donor twin has less volume and produces less urine, which causes a small amniotic sac. Other complications may occur, including:
- Weighing less than expected, a complication is known as intrauterine growth restriction (IUGR) or fetal growth restriction (FGR)
- Demise or loss of the twin
Twin to twin transfusion syndrome diagnosis
The most important step in evaluating a twin pregnancy for twin-twin transfusion syndrome is to determine whether the twins share a single placenta. An ultrasound examination early in pregnancy (during the first trimester) can best make this distinction.
Other features of TTTS include twins of the same gender, a difference in size between the twins, and a difference in the volume of amniotic fluid surrounding the two fetuses. A detailed sonographic assessment rules out any additional structural anomalies.
Twin-twin transfusion syndrome can also have a huge impact on the cardiovascular system in twins. It is important that twins with TTTS are thoroughly evaluated for heart problems while in utero.
Your evaluation will involve the following exams:
High-resolution ultrasound – An examination to rule out structural abnormalities in the twins. This exam will also confirm placental location and umbilical cord insertions into the placenta, assess amniotic fluid levels in each sac and assess blood flow patterns in specific blood vessels for each twin.
Fetal echocardiogram – A focused ultrasound of each twin’s heart to look for any related heart conditions. Twin-twin transfusion syndrome may cause serious cardiac strain in the recipient twin, resulting in enlargement of the heart and cardiac dysfunction. All twins evaluated for TTTS should undergo a fetal echocardiogram.
Genetic amniocentesis – A procedure in which a small amount of amniotic fluid is removed from the sacs surrounding the fetuses and tested. In some cases, this genetic test may be needed if imaging studies identify structural malformations in addition to TTTS.
Accurate diagnosis is extremely important in distinguishing TTTS from other related anomalies, such as selective intrauterine growth restriction (sIUGR). TTTS and sIUGR can both occur in monochorionic, diamniotic pregnancies, but are differentiated by the lack of polyhydramnios/oligohydramnios in sIUGR. The management of the two conditions are different, and therefore it is important to have a thorough evaluation to determine the most accurate diagnosis.
Treatment options for twin to twin transfusion syndrome
TTTS treatment before birth
The key to twin to twin transfusion syndrome treatment is early diagnosis and intervention. What treatment option will be best for your babies will depend on the stage of the TTTS and your babies’ gestational age at diagnosis. Several options are available, including the following:
Expectant management: This involves continued close ultrasound surveillance throughout the pregnancy. We currently recommend expectant management for most Stage 1 TTTS.
Amnioreduction: This is a procedure that is used to remove excess fluid that has accumulated in the amniotic sac of the recipient twin. The procedure is similar to that of amniocentesis, with the doctor using “real-time” ultrasound images to guide a long, very fine needle into the uterus to withdraw the fluid. We may recommend this intervention for Stage 1 TTTS or when the TTTS is diagnosed later in the pregnancy and fetoscopic laser photocoagulation (see below) is no longer an option.
Fetoscopic laser photocoagulation: This minimally invasive surgery uses a laser to ablate (seal) blood vessels that are contributing to the abnormal flow of blood to the babies (Figures 3-5). Many studies have demonstrated that this procedure for the treatment of twin to twin transfusion syndrome is the most effective therapy for babies with advanced TTTS.
Delivery: If TTTS is discovered later in the pregnancy, delivery of the babies may be the best option.
TTTS treatment after birth
Most babies with TTTS are born prematurely, but our goal will be to have your babies delivered as close to your due date as possible. Babies who are treated with laser ablation are typically delivered around week 31 or 32 of the pregnancy.
We will recommend that your babies be born at one of our specialized mother-baby centers. Children’s Minnesota is one of only a few centers nationwide with the birth center located within the hospital complex. This means that your babies will be born just a few feet down the hall from our newborn intensive care unit (NICU). If necessary, many of the physicians you have already met may be present during or immediately after your babies’ birth so we can care for them right away.