Definition
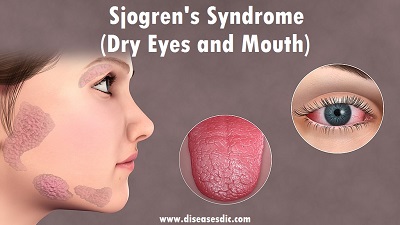
Sjogren’s syndrome is an autoimmune disease characterized by dryness of the mouth and eyes. Autoimmune diseases feature the abnormal production of extra antibodies in the blood that are directed against various tissues of the body. The misdirected immune system in autoimmunity tends to lead to inflammation of tissues. This particular autoimmune illness features inflammation and dysfunction in glands of the body that are responsible for producing tears and saliva. Inflammation of the glands that produce tears (lacrimal glands) leads to decreased water production for tears and dry eyes. Inflammation of the glands that produce the saliva in the mouth (salivary glands, including the parotid glands) leads to decreased saliva production and dry mouth and dry lips.
Sjogren’s syndrome with gland inflammation (resulting in dry eyes and mouth, etc.) that is not associated with another connective tissue disease is referred to as primary Sjogren’s syndrome. Sjogren’s syndrome that is also associated with a connective tissue disease, such as rheumatoid arthritis, systemic lupus erythematosus, or scleroderma, is referred to as secondary Sjogren’s syndrome. Dryness of eyes and mouth, in patients with or without Sjogren’s syndrome, is sometimes referred to as sicca syndrome.
Types of Sjogren’s syndrome
There are two forms of Sjogren’s syndrome:
The primary disease occurs when you experience dry eyes and a dry mouth. Fatigue and joint pain can also accompany the sicca symptoms.
The secondary disease occurs when you experience dry eyes, a dry mouth, and another associated autoimmune disease. Sjogren’s syndrome may precede lupus by many years; however, it more often occurs late in the course of lupus. Sjogren’s syndrome occurs in approximately 1-3% of the general population, but in 20-30% of people with lupus. Rheumatoid arthritis and scleroderma can also be associated with Sjogren’s syndrome.
Sjogren’s syndrome risk factors
Sjogren’s syndrome typically occurs in people with one or more known risk factors, including:
Age: Sjogren’s syndrome is usually diagnosed in people older than 40.
Sex: Women are much more likely to have Sjogren’s syndrome.
Rheumatic disease: It’s common for people who have Sjogren’s syndrome to also have a rheumatic disease such as rheumatoid arthritis or lupus.
Sjogren’s syndrome with gland inflammation
Causes of Sjogren’s syndrome
Sjögren’s syndrome is an autoimmune disease, which means something triggers your immune system to attack healthy cells. This attack damages the tear system in your eyes and the salivary glands in your mouth.
Exactly what causes this abnormal immune system response is not clear. These factors may play a role:
- Environmental factors.
- Sex hormones (the condition affects more women than men).
- Viral infections.
Symptoms
The symptoms vary greatly between individuals and may include:
- Dry eyes and few or no tears: the most frequent complaint is the sensation of a foreign body in the eye. Redness, burning, light sensitivity, eye fatigue and itching may also be present.
- Dry mouth: including difficulty chewing, swallowing food or speaking. Ulceration of the tongue and cheek membranes, a burning feeling on the tongue, altered taste sensation and the need to frequently drink fluids are common.
- Bacterial overgrowth in the mouth: saliva is important for its antibacterial function, so without adequate saliva, dental decay, periodontal disease and oral yeast infections may develop.
- Dry ear and nose: this may result in Eustachian problems of the middle ear or crusts, bleeds and a reduced sense of smell.
- Fatigue and/or depression.
- Vaginal dryness.
- Swelling and pain in the joints.
- Numbness and pins and needles.
- Muscle weakness.
- Nausea, vomiting, early satiety and abdominal bloating.
- Kidney stones.
Symptoms of Sjogren’s syndrome
Complications
Since you don’t have enough saliva, which helps protect your teeth from decay, there’s a chance you may get more cavities than other people. You could also get inflammation of your gums, called gingivitis, or yeast infections in your mouth. You also may find it hard to swallow. Dryness in your nose can lead to issues like nosebleeds or sinusitis.
Dry eyes can make you more likely to get infections around your eyes that can harm your cornea. You also may notice some new issues with your vision.
Other less common health conditions linked to Sjogren’s include:
- Irritable bowel syndrome (IBS)
- Interstitial cystitis
- Problems with your liver, like chronic active autoimmune hepatitis or primary biliary cholangitis
- Conditions that affect your lungs, like bronchitis or pneumonia
- Inflammation in your lungs, liver, and kidneys
- Lymphoma, or cancer of the lymph nodes
- Nerve issues
What kind of doctor treats Sjogren’s syndrome?
Rheumatologists have primary responsibility for managing Sjögren’s syndrome. Ophthalmologists, dentists and other specialists also can treat symptoms related to Sjögren’s.
During the years prior to diagnosis, depending on the symptoms, a person might see a number of doctors, any of whom may diagnose the disease and be involved in treatment. Usually, a rheumatologist (a doctor who specializes in diseases of the joints, muscles and bones) will coordinate treatment among a number of specialists. Other doctors who may be involved include:
- Allergist
- Dentist
- Dermatologist (skin specialist)
- Gastroenterologist (digestive disease specialist)
- Gynecologist (women’s reproductive health specialist)
- Neurologist (nerve and brain specialist)
- Ophthalmologist (eye specialist)
- Otolaryngologist (ear, nose, and throat specialist)
- Pulmonologist (lung specialist)
- Urologist
Diagnosis and test
Your doctor may do several things to find out if you have Sjogren’s syndrome. Some of the tests you may undergo include:
Physical examination
Your doctor will ask you to describe your symptoms and will look for other symptoms such as red itchy eyes; swollen salivary glands; a dry cracked tongue; and enlarged lymph glands in your neck.
Blood tests
Tests for specific blood markers can determine if you have Sjogren’s syndrome. However not everyone with Sjogren’s has these markers.
Diagnostic tests
Schirmer test: This helps determine how dry your eyes may be. It involves placing a small piece of filter paper under the lower eyelid to measure the amount of tears your eyes produce.
Slit-lamp examination: his is a more accurate way to find out if your eyes are dry. In this test the doctor puts a drop of dye into your eye and examines the eye with a special instrument called a slit lamp. The dye will stain dry or eroded areas of the eye. This test is often done by an ophthalmologist (eye doctor}.
Lip biopsy: In this test the doctor removes a few salivary glands from inside your lip. The tissue is examined under a microscope. The appearance of the tissue helps determine if you have Sjogren’s syndrome.
Salivary function tests: These measure the actual amount of saliva you produce to help determine if you have Sjogren’s.
Urine tests: These may be done to test your kidney function.
Chest X-ray: This can help detect changes in your lungs.
Treatment
Sjogren’s treatment aims to lubricate the affected areas and prevent the onset of complications.
Treatment options include:
Medications to stimulate saliva flow: These include pilocarpine and cevimeline. They have a short-term impact, limited to a few hours only, so several doses a day are usually required.
Artificial saliva: Saliva substitutes and mouth-coating gels can relieve dryness of the mouth. They are available as sprays, pre-treated swabs, and liquids. These can be important at night, as the mouth becomes dryer during sleep.
Artificial tears: Artificial tears can help to lubricate the eyes, and are available over-the-counter (OTC). Prescription options are available that reduce the need for artificial tears, such as cyclosporine ophthalmic emulsion and hydroxypropyl cellulose pellets.
Prescription eye drops: These include cyclosporine and lifitegrast.
Moisture chamber spectacles: These are special glasses that keep out irritants and retain moisture.
Prescription expectorants and throat medications: In cases of respiratory dryness, drugs such as those used to stimulate saliva flow, as well as linseed extract, sorbitol, xylitol, or malic acid, can moisturize the area.
Nonsteroidal anti-inflammatory drugs (NSAIDs): Anti-inflammatory drugs such as aspirin, naproxen, and ibuprofen can provide relief for people with Sjogren’s who are experiencing joint pain.
Disease-modifying antirheumatic drugs (DMARDs): In cases where the joint pain is accompanied by fatigue and rashes, DMARDs may relieve symptoms. Examples include hydroxychloroquine or methotrexate. If Sjogren’s seems to be affecting the muscles, nerves, lungs, or kidneys, stronger DMARDs, corticosteroids, or rituximab may be prescribed.
Antifungal medication: If oral yeast infections are occurring, medication may be prescribed to combat the fungus.
Vaginal lubricants: For vaginal dryness, water-based vaginal lubricants can provide a solution, especially during sexual intercourse.
Punctual occlusion: When all conservative treatment options have been exhausted, this surgical option seals the tear ducts with small plugs to reduce the drainage of tears from the eye. This keeps the eye moist for longer. Temporary silicone plugs are likely to be used until the procedure is confirmed successful.
Autologous eye serum: In severe cases of eye dryness, eye drops can be made from the person’s blood serum.
Here are some easy ways to keep the mouth lubricated:
- Consuming more liquids.
- Rinsing the mouth regularly to prevent infection and soothe the area
- Maintaining excellent oral and dental hygiene
- Topical fluoride gels or varnish
- Quitting smoking, as smoke irritates the mouth and speeds up the evaporation of saliva
- Chewing sugar-free gum, which stimulates the production of saliva
- Applying coconut oil to the dry areas, as it is both moisturizing and anti-microbial
Prevention
There are no known ways to prevent Sjogren’s syndrome, but these steps may help ease symptoms:
- Drink more fluids, especially water.
- Chew sugarless gum or use hard candies to moisten your mouth.
- Regularly use artificial tears and ointments to keep your eyes moistened.
- Use saline spray for your nose.
- Install a humidifier to help reduce dry eyes, nose, mouth and skin.
- Tell your eye doctor about any drugs you are taking, because some, such as antihistamines for allergies, can cause dryness.
- Use vaginal lubricants if needed.
- Don’t smoke, and avoid alcohol.