Overview – Nasal Polyps
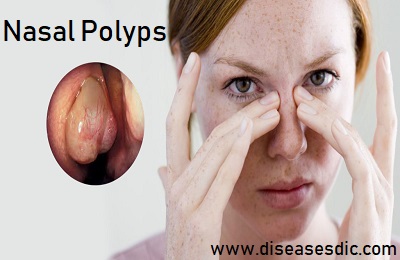
Nasal polyps are soft, painless, noncancerous growths on the lining of your nasal passages or sinuses. They hang down like teardrops or grapes. They result from chronic inflammation and are associated with asthma, recurring infection, allergies, drug sensitivity or certain immune disorders.
Small nasal polyps may not cause symptoms. Larger growths or groups of nasal polyps can block your nasal passages or lead to breathing problems, a lost sense of smell and frequent infections.
Nasal polyps can affect anyone, but they’re more common in adults. Medications can often shrink or eliminate nasal polyps, but surgery is sometimes needed to remove them. Even after successful treatment, nasal polyps often return.
Types of Nasal Polyps
There are two types.
- Antrochoanal polyps are less common and originate in the maxillary sinuses.
- Ethmoidal polyps are the most common type of nasal polyps. These polyps develop from the ethmoidal sinuses.
Pathophysiology of Nasal Polyps
The true cause is unknown, but they are thought to be due to recurrent infection or inflammation. Polyps arise from the lining of the sinuses. Nasal mucosa, particularly in the region of the middle meatus becomes swollen due to the collection of extracellular fluid. This extracellular fluid collection causes polyp formation and protrusion into the nasal cavity or sinuses. Polyps which are sessile in the beginning become pedunculated due to gravity.
In people with nasal polyps due to aspirin or NSAID sensitivity, the underlying mechanism is due to disorders in the metabolism of arachidonic acid. Exposure to cyclooxygenase inhibitors such as aspirin and NSAIDs leads to shunting of products through the lipoxygenase pathway leading to increased production of products that cause inflammation. In the airway, these inflammatory products lead to symptoms of asthma such as wheezing as well as nasal polyp formation.
What are the causes of nasal polyps?
Nasal polyps grow in the inflamed tissue of the nasal mucosa. The mucosa is a very wet layer that helps protect the inside of your nose and sinuses and humidifies the air you breathe. During an infection or allergy-induced irritation, the nasal mucosa becomes swollen and red, and it may produce fluid that drips out. With prolonged irritation, the mucosa may form a polyp. A polyp is around growth (like a small cyst) that can block nasal passages.
Although some people can develop polyps with no previous nasal problems, there’s often a trigger for developing polyps. These triggers include:
- Chronic or recurring sinus infections
- Asthma
- Allergic rhinitis (hay fever)
- Cystic fibrosis
- Churg-Strauss syndrome
- Sensitivity to nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or aspirin
There may be a hereditary tendency for some people to develop polyps. This may be due to the way their genes cause their mucosa to react to inflammation.
Risk factors
Any condition that triggers long-term irritation and swelling (inflammation) in your nasal passages or sinuses, such as infections or allergies, may increase your risk of developing polyps.
Conditions often associated with nasal polyps include:
- Asthma, a disease that causes the airway to swell (inflame) and narrow
- Aspirin sensitivity
- Allergic fungal sinusitis, an allergy to airborne fungi
- Cystic fibrosis, a genetic disorder that results in abnormally thick, sticky fluids in the body, including thick mucus from nasal and sinus linings
- Churg-Strauss syndrome (eosinophilic granulomatosis with polyangiitis), a rare disease that causes the inflammation of blood vessels
- Vitamin D deficiency, which occurs when your body doesn’t have enough vitamin D
Your family history also may play a role. There’s some evidence that certain genetic variations associated with immune system function make you more likely to develop nasal polyps.
Symptoms
If you have any symptoms, they may include:
- Stuffy or blocked nose
- Sneezing
- Postnasal drip
- Runny nose
- Facial pain
- The trouble with a sense of smell
- Loss of taste
- Itching around the eyes
- Infections
Most people with nasal polyps have a runny nose, sneezing, and postnasal drip. About 75% have problems with their sense of smell.
Many people also have wheezing, sinus infections, and sensitivity to fumes, odors, dust, and chemicals. It’s less common, but some people with nasal polyps also have a severe allergy to aspirin and reaction to yellow dyes. If you know you have that allergy, ask your doctor to check for nasal polyps.
Nasal polyps make you more likely to have long-term (chronic) sinusitis. Large ones can even change the shape of your nose.
What are the complications of nasal polyps?
The complications of nasal polyps include:
- Chronic (long-term) or frequent sinus infections
- Obstructive sleep apnea
- Asthma flare-ups
- Double vision (severe cases)
Diagnosis of Nasal polyps
Your doctor can usually make a diagnosis based on your answers to questions about your symptoms, a general physical exam and an examination of your nose. Polyps may be visible with the aid of a simple lighted instrument.
Other diagnostic tests include:
Nasal endoscopy. A narrow tube with a lighted magnifying lens or tiny camera (nasal endoscope) enables your doctor to perform a detailed examination inside your nose and sinuses.
Imaging studies. Images obtained with computerized tomography (CT) can help your doctor pinpoint the size and location of polyps in deeper areas of your sinuses and evaluate the extent of swelling and irritation (inflammation).
These studies may also help your doctor rule out other possible blockages in your nasal cavities, such as structural abnormalities or another type of cancerous or noncancerous growth.
Allergy tests. Your doctor may suggest skin tests to determine if allergies are contributing to chronic inflammation. With a skin prick test, tiny drops of allergy-causing agents (allergens) are pricked into the skin of your forearm or upper back. Your doctor or nurse then observes your skin for signs of allergic reactions.
If a skin test can’t be performed, your doctor may order a blood test that screens for specific antibodies to various allergens.
Test for cystic fibrosis. If you have a child diagnosed with nasal polyps, your doctor may suggest testing for cystic fibrosis, an inherited condition affecting the glands that produce mucus, tears, sweat, saliva and digestive juices.
The standard diagnostic test for cystic fibrosis is a noninvasive sweat test, which determines whether your child’s perspiration is saltier than most people’s sweat is.
Blood test. Your doctor may test your blood for low levels of vitamin D, which are associated with nasal polyps.
Treatment of nasal polyps
The goal of nasal polyps’ treatment is to reduce the inflammation that causes the polyps. When the inflammation is reduced the polyps become smaller or sometimes even disappear. If polyps do not sufficiently shrink or disappear surgery may be necessary. The use of medication represents the first-line treatment, and surgery (=polyps removal) is recommended as second-line treatment.
Medications
- Nasal corticosteroids: Corticosteroid nasal sprays are generally prescribed to reduce the inflammation. This treatment may shrink the polyps or eliminate them.
- Oral corticosteroids: If a nasal corticosteroid is not effective, an oral corticosteroid may be prescribed. Because oral corticosteroids can cause serious side effects, they are generally taken only for a limited period of time.
- Antibiotics: Antibiotics may be prescribed in case of chronic and recurring infection of your sinuses. Some antibiotics also have anti-inflammatory properties which may reduce the inflammation of your sinuses as well as the size of the polyp.
- Antihistamines: If you suffer from allergies, antihistamines may be prescribed to help to reduce the allergic inflammation of your sinuses and nose.
- Biologicals: Biological drugs are promising novel treatments (new molecules) currently being tested to reduce the size of polyps in patients with chronic rhinosinusitis.
Surgery
The standard procedure to remove nasal polyps is Functional Endoscopic Sinus Surgery (FESS). The surgeon will insert a small tube with a tiny camera into the nostrils and guide it into the sinus cavities and the polyps will be removed. During the operation, the surgeon may also remove the disease in additional key areas in order to restore adequate aeration and drainage of the sinuses. Endoscopic surgery is usually performed as an outpatient procedure.
Note that even after surgical removal of the nasal polyps, the inflammation may still remain. Therefore, to improve your smell it is important to continue your medications because they reduce the inflammation of the olfactory mucosa.
Why do nasal polyps grow back after surgery?
Chronic rhinosinusitis with nasal polyps is a chronic disease. This condition will need constant treatment with corticosteroids to prevent the worsening of the symptoms. Unfortunately, in some cases, even the nasal sprays with corticosteroids are not strong enough to suppress the polyp growth.
How do I prevent it?
Not everyone will be able to prevent. However, there are a few ways you may be able to help yourself. The strategies include the following:
- Follow your doctor’s instructions on taking your allergy and asthma medications.
- Avoid breathing airborne allergens or irritants that lead to inflammation of your nose and sinus cavities.
- Practice good hygiene.
- Use a humidifier in your home to help moisten your breathing passages.
- Use a saline nasal rinse or spray to remove allergens or other irritants.