Definition – Ichthyosis
Ichthyosis is a generalized, mostly genetic disorder of the skin. All types of ichthyosis have dry, thickened, scaly or flaky skin. There is no cure, but symptoms are usually mild and manageable with a daily skincare routine. The severity of symptoms can vary extremely, from the mildest types such as ichthyosis vulgaris which may be mistaken for normal-dry skin up to life-threatening conditions such as harlequin type ichthyosis. The most common type of ichthyosis is ichthyosis vulgaris, accounting for more than 95% of cases.
Epidemiology
Incidence and prevalence rates vary depending on the type of ichthyosis and the population studied. The prevalence of ichthyosis vulgaris, the most common form of ichthyosis, was determined to be about 1 in 250 individuals in a UK population, and 2.29% in the Chinese population. X-linked ichthyosis occurs in about 1 in 2000 to 6000 males. The other primary ichthyoses, autosomal recessive congenital ichthyosis, and epidermolytic ichthyosis, occur much less frequently, with an estimated prevalence of about 1 in 300,000.
Types
Ichthyosis Vulgaris – Patients experience dryness of the skin and mild scaling.
Epidermolytic Ichthyosis or Epidermolytic Hyperkeratisis – Patients afflicted with Epidermolytic ichthyosis will find spiny dark thick scales forming on the skin and the skin may also be prone to blistering under almost any kind of impact or trauma.
Lamellar Ichthyosis – Thickening of the skin is again present in this variation of ichthyosis, but one would also observe the formation of large, plate-like scales.
Congenital Ichthyosiform Erythroderma- In addition to scaly, dry skin, redness and inflammation are also observed.
Localized Ichthyosis – In this type, the thickening and scaly appearance of the skin is not present across the entire body, but is restricted to specific regions such as the foot soles or palms of the hand.
Risk factors
The following factors can increase the risk of a person to develop ichthyosis:
- A family history of the condition
- Exposure to dry or cold environments
Causes
- Most known forms of ichthyosis are hereditary disorders. Some forms are caused by dominant genes; some are caused by recessive genes.
- In some forms of ichthyosis, the skin cells are produced at the normal rate, but they do not separate normally at the surface of the outermost layer of skin (stratum corneum) and are not shed as quickly as they should be.
- In other forms, there is an overproduction of skin cells in the epidermis. The cells reach the stratum corneum in as few as four days, compared to the normal fourteen.
- New cells are made faster than the old cells are shed and build up in the stratum corneum and underlying layers. The result in both instances is a build-up of scale.
Signs and Symptoms
Symptoms include thick, scaly, dry and cracked skin. If your child has ichthyosis, their skin may appear normal at birth, but then gradually dry out and become scaly. Symptoms usually appear by the age of five years.
- All parts of the body can be affected, including the face and scalp; however, the bends in the arms and legs are not usually affected. The palms and soles tend to have very thick skin.
- Most children will have a mild form of the disease, and there will a minimal effect on their general health and wellbeing.
- Some children will find the condition uncomfortable or embarrassing.
- In rare cases, it can be very severe and affect the entire skin surface or cause blisters. In this case, repeated infections, discomfort, and sweating problems may occur.
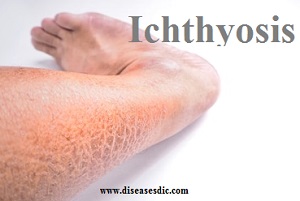
Severe scaling on the leg
Ichthyosis complications
Some people may experience:
Overheating: In rare cases, the skin thickness and scales of ichthyosis can interfere with sweating. This can inhibit cooling. In some people, excess sweating (hyperhidrosis) can occur.
Secondary infection: Skin splitting and cracking may lead to infections.
Diagnosis and test
It is a clinical diagnosis. Genetic testing is available in some centers. Prenatal testing may be available for X-linked ichthyosis.
Recessive X-linked ichthyosis is confirmed by absent steroid sulphatase in fibroblasts and elevated plasma cholesterol sulfate levels.
Biopsy reveals:
- Thick, hyperkeratotic stratum corneum
- Reduced or absent granular cell layer and filaggrin in ichthyosis vulgaris
- Lamellar body ‘ghosts’ in lamellar ichthyosis
- Vacuolar degeneration of suprabasal keratinocytes and coarse keratohyalin granules in thickened granular layer in keratinopathic ichthyosis
Treatment and medications
- The treatment involves a restoration of the person’s skin moisture, as well as facilitation of more aggressive shedding of dead skin cells.
- People with the disease may choose to visit a dermatologist on a regular basis to help with Ichthyosis should it cause them severe symptoms.
- Use of moisture-retaining creams or ointments after bathing or showering can help people affected by the disease to keep moisture within their skin’s surface.
- Products that contain lanolin, urea, or petrolatum are very helpful in the maintenance of skin moisture.
- There are creams or lotions containing medicines which promote the shedding of skin flakes. These creams or lotions contain lactic acid or other alpha hydroxy acids.
- People affected may need to use antibiotics on occasion if scratching causes skin infection, or if body odor becomes a major problem.
- It is important for people with the disease to contact a health care provider if they develop either a fever, or redness of the skin, because ichthyosis may make their skin a less-effective barrier to infection.
- It is something that is very manageable with effective and continued treatment. Some types of the disease improve after the person grows out of childhood.
- There are some forms of the disease they may be life-threatening, even in infancy, should the person’s skin problems become severe.
Prevention
There is no way to prevent ichthyosis. As with other genetic diseases, there is a risk that children of an affected parent will inherit the gene.