Overview – Blastomycosis
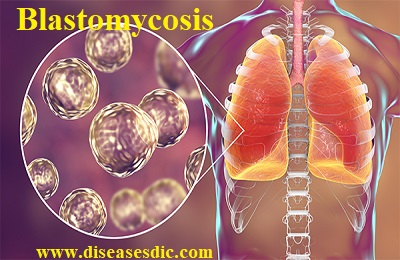
Blastomycosis is a systemic pyogranulomatous infection usually caused by the inhalation of (spores) conidia of Blastomyces dermatitidis. Clinical presentations vary widely, ranging from an asymptomatic, self-limited pulmonary infection to acute respiratory distress syndrome (ARDS), a life-threatening disease. Blastomycosis is not known to spread from person to person.
Pathogenesis of Blastomycosis
Inhaled conidia of B. dermatitidis are phagocytosed by neutrophils and macrophages in alveoli. Some of these escape phagocytosis and transform into yeast phase rapidly. Having thick walls, these are resistant to phagocytosis and express glycoprotein, BAD-1, which is a virulence factor as well as an epitope. In lung tissue, they multiply and may disseminate through blood and lymphatics to other organs, including the skin, bone, genitourinary tract, and brain. The incubation period is 30 to 100 days, although infection can be asymptomatic.
What Causes Blastomycosis?
Blastomycosis is caused when the spores of the offending fungus Blastomyces Dermatitidis become airborne and inhaled by an individual. Although most of the fungus is killed when they enter the lungs by specialized cells present in the lungs, there are some spores that take the form of yeast like infection and are not able to be destroyed by these cells. This happens basically because of the body temperature which changes the form of spores from fungal to yeast. These yeasts then start to multiply and spread to other organs and parts of the body through the blood resulting in Blastomycosis.
What Are the Risk Factors for Blastomycosis?
Although almost anyone can become infected with the fungi, those at the highest risk for blastomycosis are immunosuppressed individuals and those that live in or visit areas where the fungal spores are plentiful. Since the fungi prefer damp forested areas, people who are hunters, forestry workers, campers, and farmers are at higher risk to get blastomycosis. Blastomycosis cannot be spread from person to person or animal to person.
Symptoms
Lung infection may not cause any symptoms. Symptoms may be seen if the infection spreads. Symptoms may include:
- Joint pain
- Chest pain
- Cough (may produce brown or bloody mucus)
- Fatigue
- Fever and night sweats
- General discomfort, uneasiness, or ill feeling (malaise)
- Muscle pain
- Unintentional weight loss
Most people develop skin symptoms when the infection spreads. You may get papules, pustules, or nodules on exposed body areas.
The pustules:
- May look like warts or ulcers
- Are usually painless
- Vary in color from gray to violet
- May appear in the nose and mouth
- Bleed easily and form ulcers
Possible Complications of Blastomycosis
Complications of blastomycosis may include:
- Large sores with pus (abscesses)
- Skin sores can lead to scarring and loss of skin color (pigment)
- Return of the infection (relapse or disease recurrence)
- Side effects from drugs such as amphotericin B
Diagnosis and test
Patient History
Patient history is also important in the diagnosis, particularly in areas where there may be a disease outbreak.
Test and screening
- Fungal cultures and smear
- Blastomyces urine antigen
If blastomycosis is suspected, a chest x-ray should be taken. Focal or diffuse infiltrates may be present, sometimes as patchy bronchopneumonia fanning out from the hilum. These findings must be distinguished from other causes of pneumonia (eg, other mycoses, tuberculosis [TB], tumors).
Skin lesions can be mistaken for sporotrichosis, TB, iodism, or basal cell carcinoma. Genital involvement may mimic TB.
Cultures of infected material are done; they are definitive when positive. Because culturing Blastomyces can pose a severe biohazard to laboratory personnel, the laboratory should be notified of the suspected diagnosis. The organism’s characteristic appearance, seen during the microscopic examination of tissues or sputum, is also frequently diagnostic.
Serologic testing is not sensitive but is useful if positive.
A urine antigen test is useful, but cross-reactivity with Histoplasma is high.
Molecular diagnostic tests (eg, polymerase chain reaction [PCR]) are becoming available.
How is Blastomycosis treated?
Approach Considerations
Not all patients with Blastomycosis require treatment. Occasionally the symptoms from Blastomycosis may go away without treatment. People with evidence of Blastomycosis spreading beyond the lungs, or whose symptoms do not improve, will require treatment. The type of treatment you will be given depends on how severe your symptoms are and whether you are immunosuppressed (have a weakened immune system).
Antifungal Treatments
Treatment of blastomycosis depends on severity of the infection.
Mild to moderate disease: itraconazole 200 mg orally 3 times a day for 3 days, followed by 200 mg orally once a day or 2 times a day for 6 to 12 months is used. Fluconazole appears less effective, but 400 to 800 mg orally once a day may be tried in itraconazole-intolerant patients with mild disease.
Severe, life-threatening infections: IV amphotericin B is usually effective. The Infectious Diseases Society of America’s guidelines recommends a lipid formulation of amphotericin B at a dosage of 3 to 5 mg/kg once a day or amphotericin B deoxycholate 0.7 to 1.0 mg/kg once a day for 1 to 2 weeks or until improvement is noted.
Therapy is changed to oral itraconazole once patients improve; dosage is 200 mg 3 times a day for 3 days, then 200 mg 2 times a day for ≥ 12 months.
Patients with central nervous system blastomycosis, pregnant patients, and immunocompromised patients should be treated with IV amphotericin B (preferably liposomal amphotericin B), using the same dose schedule as for life-threatening infection.
Voriconazole, isavuconazole, and posaconazole are active against B. dermatitidis, but clinical data are limited, and the role of these drugs has not yet been defined.
Are there Home Remedies for Blastomycosis?
Blastomycosis should not be attempted at home; a physician needs to diagnose, treat, and follow up with the infected patient to be sure the patient has adequate treatments and does not relapse.
Prevention
- Unfortunately, there are no known practical measures for the prevention of blastomycosis.
- There are currently no methods to test soil for the presence of Blastomyces species.
- Illness caused by blastomycosis can be minimized by early recognition and appropriate treatment of the disease. Awareness of the disease by both the public and health care providers is the key to early diagnosis.