Definition
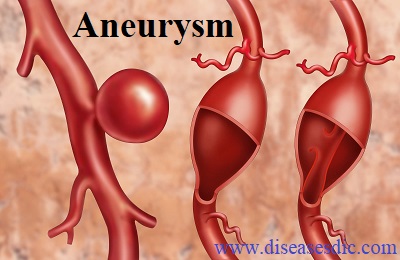
An aneurysm occurs when an artery’s wall weakens and causes an abnormally large bulge. This bulge can rupture and cause internal bleeding. About 13,000 deaths occur each year in the United States from aortic aneurysms. Although an aneurysm can occur in any part of your body, they’re most common in the:
- Brain
- Aorta
- Legs
- Spleen
Brief history about Aneurysm
Earliest records of abdominal aorta aneurysm in history come from Ancient Rome in the 2nd century AD. Greek surgeon Antyllus tried to treat the aneurysm with proximal and distal ligature, central incision and removal of thrombotic material from the aneurysm. The surgical management of aneurysms however dates back to 3000 years.
Surgical history of Aneurysm
Surgery was unsuccessful until 1923. In that year, Rudolph Matas performed the first successful aortic ligation on a human. Other non-conventional methods that were tried included wrapping the aorta with polyethene cellophane, which induced fibrosis and restricted the growth of the aneurysm. Over the course of surgical history arose three landmark developments in aortic surgery. These were:
- Ligation or tying up of the aorta
- Open repair of the bulging artery
- Endovascular repair of the artery
Epidemiology about aneurysm
The prevalence of AAA varies with a number of factors, including advancing age, family history, gender and tobacco use. The prevalence of AAAs larger than 2.9 cm in diameter ranges from 1.9% to 18.5% in men and 0% to 4.2% in women, the ranges being explained by the different age groups used and the differences in case-mix.
The prevalence of AAAs in women is currently considered too low for their inclusion in ultrasonographic screening programmes and stratified analyses in the various RCTs. Wanhainen recently demonstrated that prevalence in women is underestimated by using the standard definition for AAA of a 30 mm diameter. The prevalence for 65–75-year-old was 16.9% for men and 3.5% for women, whereas when using another definition, ≥1.5 × normal infrarenal aortic diameter (predicted from a nomogram), the prevalence was 12.9% for men and 9.8% for women.
Types of Aneurysms
Abdominal aortic aneurysm
An aortic aneurysm is a weakened or bulging area on the wall of the aorta. An abdominal aortic aneurysm occurs when the large blood vessel (the aorta) that supplies blood to the abdomen, pelvis and legs becomes abnormally large or balloons outward. This type of aneurysm is most often found in men over age 60 who have at least one or more risk factor, including emphysema, family history, high blood pressure, high cholesterol, obesity and smoking. The rupture of an abdominal aortic aneurysm is a medical emergency, and only about 20 percent of patients survive.
An aortic aneurysm is a weakened or bulging area on the wall of the aorta.
Symptoms of abdominal aortic aneurysm includes:
- Chest pain and Jaw pain, are generally associated with a heart attack, but the sudden stabbing, radiating pain, fainting, difficulty breathing, and sometimes even sudden weakness on one side are also symptoms of an aortic event.
Cerebral Aneurysm or Brain Aneurysm
Cerebral aneurysms, which affect about 5 percent of the population, occur when the wall of a blood vessel in the brain becomes weakened and bulges or balloons out. There are many types of aneurysms. The most common, a “berry aneurysm,” is more common in adults. It can range in size from a few millimeters to more than a centimeter. A family history of multiple berry aneurysms may increase your risk.
Conditions that injure or weaken the walls of the blood vessel, including atherosclerosis, trauma or infection, may also cause cerebral aneurysms. Other risk factors include medical conditions such as polycystic kidney disease, narrowing of the aorta and endocarditis. Like other types of aneurysm, cerebral aneurysms may not have any symptoms. Symptoms may include:
- Severe headache
- Double vision
- Loss of vision
- Headaches
- Eye pain
- Neck pain
- Stiff neck
- Thoracic Aortic Aneurysm
A thoracic aortic aneurysm is an abnormal bulging or ballooning of the portion of the aorta that passes through the chest.
The most common cause is atherosclerosis, or hardening of the arteries. Other risk factors include:
- Aging
- Genetic conditions, such as Marfan syndrome
- Inflammation of the aorta
- Injury from falls or other trauma
- Syphilis
A patient with an aneurysm may not experience any symptoms until the aneurysm begins to “leak” blood into nearby tissue or expand. Symptoms of a thoracic aortic aneurysm may include:
- Hoarseness
- Swallowing problems
- High-pitched breathing
- Swelling in the neck
- Chest or upper back pain
- Clammy skin
- Nausea and vomiting
- Rapid heart rate
- Sense of impending doom
Causes
A person may inherit the tendency to form aneurysms, or aneurysms may develop because of hardening of the arteries (atherosclerosis) and aging. The following risk factors may increase your risk for an aneurysm or, if you already have an aneurysm, may increase your risk of it rupturing:
- Family history. People who have a family history of aneurysms are more likely to have an aneurysm than those who don’t.
- Hardening of the arteries (atherosclerosis).Atherosclerosis occurs when fat and other substances build up on the lining of a blood vessel. This condition may increase your risk of an aneurysm.
- High blood pressure. The risk of subarachnoid hemorrhage is greater in people who have a history of high blood pressure.
- Blood vessel diseases in the aorta. Abdominal aortic aneurysms can be caused by diseases that cause blood vessels to become inflamed.
- Trauma, such as being in a car accident, can cause abdominal aortic aneurysms.
- Infection in the aorta. Infections, such as a bacterial or fungal infection, may rarely cause abdominal aortic aneurysms.
- In addition to being a cause of high blood pressure, the use of cigarettes may greatly increase the chances of a brain aneurysm rupturing.
Complications in Aneurysm
- Thromboembolism – depending on where the clot has traveled to, thromboembolism can cause pain in the extremities or the abdomen. If a clot travels to the brain, it can cause a stroke
- Dissection of the aorta – People who have an aortic dissection often describe a tearing or ripping pain in the chest that is abrupt and excruciating, and the pain can travel as the dissection progresses along the aorta. The pain can radiate toward the back.
- Severe chest and/or back pain – If a silent or diagnosed aortic aneurysm in the chest ruptures, severe chest or back pain may arise. Such symptoms may help hospital medical staff diagnose an aneurysm.
- Angina – Certain types of aneurysm can lead to angina, another type of chest pain; the pain is related to narrowed arteries supplying the heart itself (causing myocardial ischemia and possibly heart attack).
- Sudden extreme headache – If a brain aneurysm leads to subarachnoid hemorrhage (a kind of stroke), the main symptom is sudden extreme headache; often so severe that it is unlike any previous experience of head pain.
Diagnosis and test for aneurysm
- Computed tomography (CT) scan. A CT scan can help identify bleeding in the brain. Sometimes a lumbar puncture may be used if your doctor suspects that you have a ruptured cerebral aneurysm with a subarachnoid hemorrhage.
- Computed tomography angiogram (CTA) scan. CTA is a more precise method of evaluating blood vessels than a standard CT scan. CTA uses a combination of CT scanning, special computer techniques, and contrast material (dye) injected into the blood to produce images of blood vessels.
- Magnetic resonance angiography (MRA). Similar to a CTA, MRA uses a magnetic field and pulses of radio wave energy to provide pictures of blood vessels inside the body. As with CTA and cerebral angiography, a dye is often used during MRA to make blood vessels show up more clearly.
- Cerebral angiogram. During this X-ray test, a catheter is inserted through a blood vessel in the groin or arm and moved up through the vessel into the brain. A dye is then injected into the cerebral artery. As with the above tests, the dye allows any problems in the artery, including aneurysms, to be seen on the X-ray. Although this test is more invasive and carries more risk than the above tests, it is the best way to locate small (less than 5 mm) brain aneurysms.
- Abdominal ultrasound. This test is most commonly used to diagnose abdominal aortic aneurysms. During this painless exam, you lie on your back on an examination table and a small amount of warm gel is applied to your abdomen. The gel helps eliminate the formation of air pockets between your body and the instrument the technician uses to see your aorta, called a transducer. The technician presses the transducer against your skin over your abdomen, moving from one area to another. The transducer sends images to a computer screen that the technician monitors to check for a potential aneurysm.
Treatment and medications
Aortic aneurysms are treated with medicines and surgery. Small aneurysms that are found early and aren’t causing symptoms may not need treatment. Other aneurysms need to be treated. The goals of treatment may include:
- Preventing the aneurysm from growing
- Preventing or reversing damage to other body structures
- Preventing or treating a rupture or dissection
- Allowing you to continue doing your normal daily activities
Treatment for an aortic aneurysm is based on its size. Your doctor may recommend routine testing to make sure an aneurysm isn’t getting bigger. This method usually is used for aneurysms that are smaller than 5 centimeters (about 2 inches) across.
Medicines
If you have an aortic aneurysm, your doctor may prescribe medicines before surgery or instead of surgery. Medicines are used to lower blood pressure, relax blood vessels, and lower the risk that the aneurysm will rupture (burst). Beta blockers and calcium channel blockers are the medicines most commonly used.
Surgery
- Open Abdominal or Open Chest Repair: The standard and most common type of surgery for aortic aneurysms is open abdominal or open chest repair. This surgery involves a major incision (cut) in the abdomen or chest.
- Endovascular Repair: In endovascular repair, the aneurysm isn’t removed. Instead, a graft is inserted into the aorta to strengthen it. Surgeons do this type of surgery using catheters (tubes) inserted into the arteries; it doesn’t require surgically opening the chest or abdomen. General anesthesia is used during this procedure.
The surgeon first inserts a catheter into an artery in the groin (upper thigh) and threads it to the aneurysm. Then, using an x ray to see the artery, the surgeon threads the graft (also called a stent graft) into the aorta to the aneurysm. The graft is then expanded inside the aorta and fastened in place to form a stable channel for blood flow. The graft reinforces the weakened section of the aorta. This helps prevent the aneurysm from rupturing.
- Surgical clipping. This surgery involves placing a small metal clip around the base of the aneurysm to isolate it from normal blood circulation. This decreases the pressure on the aneurysm and prevents it from rupturing. Whether this surgery can be done depends on the location of the aneurysm, its size, and your general health.
Prevention
The best way to prevent an aortic aneurysm is to avoid the factors that put you at higher risk for one. They are as follows:
- Smoking is a greater risk factor for aneurysm than it is for atherosclerosis, the cardiovascular disease where fatty deposits accumulate on the arterial wall and which can weaken artery walls.
- A healthy diet includes a variety of fruits, vegetables, and whole grains. It also includes lean meats, poultry, fish, beans, and fat-free or low-fat milk or milk products. A healthy diet is low in saturated fat, Tran’s fat, cholesterol, sodium (salt), and added sugar.