What is Achilles Tendinopathy?
Achilles tendinopathy (common overuse injury) refers to a combination of pathological changes affecting the Achilles tendon usually due to overuse and excessive chronic stress upon the tendon. It can be seen both in athletes and non-athletes. It may or may not be associated with an Achilles tendon tear. A lack of flexibility or a stiff Achilles tendon can increase the risk of these injuries.
Surgical specimens show a range of degenerative changes of the affected tendon, e.g., the tendon fiber structure and arrangement; an increase in glycosaminoglycans (water-binding molecules that can hold nearly 1,000 times their own weight), which may explain the swelling of the tendon.
The precise cause of tendonitis remains unclear. Even though tendonitis of the Achilles tendon is often connected to sports activities, the ailment is also often found in people who do not practice sports. The biggest cause is the excessive overburdening of the tendon. A light degeneration of the Achilles tendon can be latently present, but the pain only appears when the tendon is overburdened. It is also noted that the ailment is usually not preceded by trauma.
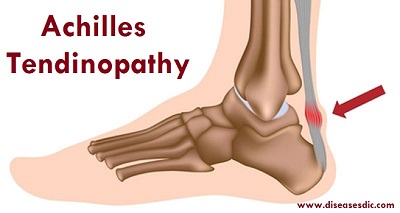
Overview and anatomy of Achilles Tendinopathy
The Achilles tendon is a thick tendon located in the back of the leg. It connects the gastrocnemius and soleus muscles in the calf to an insertion point at the calcaneus (heel bone). It is the strongest tendon in the body and allows people to push off while walking, running and jumping.
Achilles injuries can occur in several places, but the most common area is at the muscle-tendon junction – the area where the calf muscles join with the tendon. Injuries in this area often heal on their own. This junction has a smaller blood supply than does the muscular area of the leg, however. This makes the healing process slower than it is in many other leg injuries.
Epidemiology
Achilles tendinopathy is one of the most frequently ankle and foot overuse injuries. This disorder is more likely to be found in the individuals who participate in the physical activities such as running and jumping. It may affect 9% of recreational runners and cause up to 5% of professional athletes to end their careers. In an epidemiologic investigation of 1394 nonathletes, Achilles tendinopathy was found in 5.6% of the subjects (4% insertional, 3.6% noninsertional, and 1.9% both forms). In another research, Kvist found that 20% to 25% of Achilles tendinopathy patients had insertional disorder, 66% had noninsertional, and 23% had either retrocalcaneal bursitis or insertional tendinopathy.
Chronic Achilles tendinopathy is more common in older people than in young people. In Kvist’s study, among 470 patients who had Achilles tendinopathy, only 25% of the patients were young athletes and 10% were younger than 14 years. Moreover, insertional tendinopathy tends to occur in more active persons, whereas noninsertional tendon injury tends to occur in older, less active, and overweight persons.
Pathophysiology of Achilles Tendinopathy
The Achilles tendon originates from the gastrocsoleus complex and inserts onto the calcaneus distally. Histologically, it is composed of tenoblasts and tenocytes (90-95%), chondrocytes (5-10%) and some synovial cells. The extracellular matrix is made up of glycosaminoglycans, proteoglycans, and glycoproteins. Collagen accounts for 70-80% of the dry weight of the tendon and is composed primarily of type I (95%), type III, V, and XII. Elastin accounts for 2% of the dry weight; however, the tendon can undergo 200% strain before failing. Collagen forms fibrils, fibers, fascicles which come together to form bundles surrounded by an endotenon which carries the blood supply, nerves and lymphatics.
Biomechanical intrinsic factors which contribute to AT include hyperpronation of the foot, along with ankle equinus (frequently caused by pes planus). Ankle equinus is defined by ankle dorsiflexion limited to 10-20°. This causes increased foot pronation in order to gain the added benefit of increased dorsiflexion in order to maintain proper gait mechanics. This excessive hyperpronation at the subtalar joint causes the gastrocnemius-soleus complex and tibiialis posterior to eccentrically contract with greater force. This compensation occurs to decelerate the rotation of the lower extremity and pronation of the foot. The frequent forceful contraction contributes to the development of AT.
In AT, the tendon becomes thickened, brown and uneven. At the cellular level, there is an increase in the number of tenocytes, concentration of glycosaminoglycans, disorganization of the collagen fibers and neovascularization. In chronic AT, there is an increased concentration of type III collagen, fibronectin, tenascin C, aggrecan, and biglycan.
Types of Achilles Tendinopathy
There are two types of Achilles tendinitis, based on which part of the tendon is inflamed. The two types can occur separately or at the same time.
Noninsertional Achilles Tendinitis
In noninsertional Achilles tendinitis, fibers in the middle portion of the tendon (above where it attaches to the heel) are affected. Over time, the fibers may begin to break down and develop tiny tears. This can lead to tendon swelling and thickening. Noninsertional tendinitis more commonly affects younger, active people, especially runners.
Insertional Achilles Tendinitis
Insertional Achilles tendinitis involves the lower portion of the tendon, where it attaches (inserts) to the heel bone (also known as the calcaneus). In both noninsertional and insertional Achilles tendinitis, damaged tendon fibers may calcify (harden) over time. Bone spurs often form on the heel with insertional Achilles tendinitis.
Insertional Achilles tendinitis can occur at any time or activity level, although it is still most common in runners. It is frequently caused by calf muscle tightness, which places increased stress on the Achilles tendon insertion.
Severity of Achilles tendinopathy
Achilles tendinopathy is graded according to how severe it is:
- Mild – pain in the Achilles tendon during a particular activity (such as running) or shortly after.
- Moderate – the Achilles tendon may swell. In some cases, a hard lump (nodule) may form in the tendon
- Severe – any type of activity that involves weight-bearing causes pain of the Achilles tendon. Very occasionally, the Achilles tendon may rupture (tear). When an Achilles tendon ruptures, it is said to feel like a hard whack on the heel.
Causes of Achilles Tendinopathy
Achilles tendinopathy generally occurs from gradual wear and tear of the tendon due to overuse or ageing. Although it may seem like a sudden injury, it is more likely that the tendon has weakened over time from completing the same actions over and over in your job, exercise routine or even regular daily activities.
The most common causes include:
- Overuse or over-training
- Wearing poorly supported footwear while exercising or training
- Sudden change in the intensity, duration and occurrence of your training routine
- Exercising on hard or uneven surfaces
- Poor exercise or training techniques
- Tight calf muscles from lack of stretching
Symptoms
The onset of the symptoms of Achilles tendonitis tends to be gradual, usually developing over a period of several days, or even weeks. Symptoms may include:
- Pain – this may be mild at first and may only be noticeable after exercise. Over time the pain may become constant and severe
- Stiffness – this is usually relieved by activity
- Sluggishness in the leg
- Tenderness – particularly in the morning and most commonly felt just above where the tendon attaches to the heel bone
- Swelling.
Achilles Tendinopathy Risk factors
Many things affect the stress or force being put through the tendon. However, it is not simply the result of exercising too much.
General risks:
- Age: It is most common from the age of 30 onwards
- Gender: It is more common in males
- Weight: If you have a higher-than-average body mass index (BMI) you are more at risk.
- Diabetes
- Smoking
- Tight and/or weak calf muscles (the muscles in the lower part of your leg)
- Reduced endurance strength in the lower leg muscles
- Reduced strength around hips and knee muscles
- Stiff joints in your foot
Certain aspects of exercise and training can also increase your risk of developing an Achilles tendinopathy.
Common training errors include:
- Running too far when your body is not ready for this distance
- Running at too high an intensity
- Increasing running distances too soon
- Lack of variation in training
- Old or poor-quality footwear for leisure or exercise
- Too much hill running
Complications
Complications of an Achilles tendon injury may include:
- Pain, which can be severe
- Difficulty walking or being active
- Warping of your tendon area or heel bone
- Tendon rupture from reinjury
Other complications can happen because of the treatments used to care for an Achilles tendon injury. For instance:
- Sometimes cortisone injections can cause the tendon to tear
- Surgery can lead to pain and infection
Diagnosis
During the physical exam, your doctor will gently press on the affected area to determine the location of pain, tenderness or swelling. He or she will also evaluate the flexibility, alignment, range of motion and reflexes of your foot and ankle.
Imaging tests
Your doctor may order one or more of the following tests to assess your condition:
- X-rays. While X-rays can’t visualize soft tissues such as tendons, they may help rule out other conditions that can cause similar symptoms.
- Ultrasound. This device uses sound waves to visualize soft tissues like tendons. Ultrasound can also produce real-time images of the Achilles tendon in motion, and color-Doppler ultrasound can evaluate blood flow around the tendon.
- Magnetic resonance imaging (MRI). Using radio waves and a very strong magnet, MRI machines can produce very detailed images of the Achilles tendon.
Treatment
Treatment approaches for Achilles Tendinopathy are selected on the basis of how long the injury has been present and the degree of damage to the tendon. In the early stage, when there is sudden (acute) inflammation, one or more of the following options may be recommended:
Immobilization: Immobilization may involve the use of a cast or removable walking boot to reduce forces through the Achilles tendon and promote healing.
Ice: To reduce swelling due to inflammation, apply a bag of ice over a thin towel to the affected area for 20 minutes of each waking hour. Do not put ice directly against the skin.
Oral medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be helpful in reducing the pain and inflammation in the early stage of the condition.
Orthotics: For those with overpronation or gait abnormalities, custom orthotic devices may be prescribed.
Night splints: Night splints help to maintain a stretch in the Achilles tendon during sleep.
Night splints for Achilles Tendinopathy
Physical therapy: Physical therapy may include strengthening exercises, soft-tissue massage/mobilization, gait and running re-education, stretching and ultrasound therapy.
Other treatments for Achilles tendinopathy
If your Achilles tendinopathy doesn’t improve with self-help measures or physiotherapy exercises, there may be other treatments you can try. These include the following.
- Extracorporeal shockwave therapy. This is where a machine passes shockwaves through your skin to the damaged part of your tendon. This may help to ease your pain. You may need several sessions.
- Blood or platelet-rich plasma (PRP) injections. These use part of your own blood that’s rich in growth factors and may help your Achilles tendon to heal faster. Your doctor injects the plasma or blood into or around your damaged tendon, sometimes using ultrasound for guidance.
- Dry needling. This involves passing a thin needle into your tendon with the aim of triggering the healing process and strengthening your tendon.
Your physiotherapist may be able to deliver some of these therapies. But for others, you may need a referral to a specialist sports or musculoskeletal doctor. Some of these treatments may only be available in specialist centres or as part of a research trial.
Does Achilles tendinitis need surgery?
If you’ve tried nonsurgical methods for six months and you’re still in pain, talk to your provider. You may need surgery. A foot and ankle surgeon can suggest options based on your injury, age, preferences and activity level.
Surgical options include:
- Gastrocnemius recession: The surgeon lengthens the calf (gastrocnemius) muscles.
- Debridement and repair: If most of the tendon is healthy, the surgeon removes just the damaged part and stitches together the remaining healthy tendon. After the procedure, you’ll wear a boot or cast for a few weeks.
- Debridement with tendon transfer: If more than half of the Achilles tendon is damaged, then there’s not enough healthy part of the Achilles tendon to function. You need an Achilles tendon transfer. Your surgeon takes the tendon that helps the big toe point down and moves it to the heel bone. Treatment gives the damaged tendon enough strength to function. You’ll still be able to move your big toe, walk and even run. But you may not be able to play sports competitively after this procedure.
- Hydrocision TenJet®: This minimally invasive, ultrasound guided technique uses high velocity saline to break up scar tissue in the tendon. The pressurized saline acts as blade to selectively remove unhealthy tissue. This is done on an outpatient basis.
Prevention of Achilles Tendinopathy
Achilles tendinitis cannot be completely prevented, but the risk of developing it can be reduced by being aware of the possible causes and taking precautions.
These include:
- Varying exercise: Alternating between high-impact exercises, such as running, and low-impact exercise, for example, swimming, can reduce stress on the Achilles tendon on some days.
- Limiting certain exercises: Too much hill running, for example, can put excessive strain on the Achilles tendon.
- Wearing the correct shoes and replacing them when worn: Shoes that support the arch and protect the heel create less tension in the tendon.
- Using arch supports inside the shoe: This can help if the shoe is in good condition but does not provide the required arch support.
- Gradually increasing the intensity of a workout: Achilles tendinitis can occur when the tendon is suddenly put under too much strain, so warming up and increasing the level of activity gradually gives the muscles time to loosen up, and this puts less pressure on the tendon.
It is important to stretch and warm up before and after exercising. Stretching helps to keep the Achilles tendon flexible, so there is less chance of tendinitis developing. Stretching every day, including rest days, will further improve flexibility.