Overview
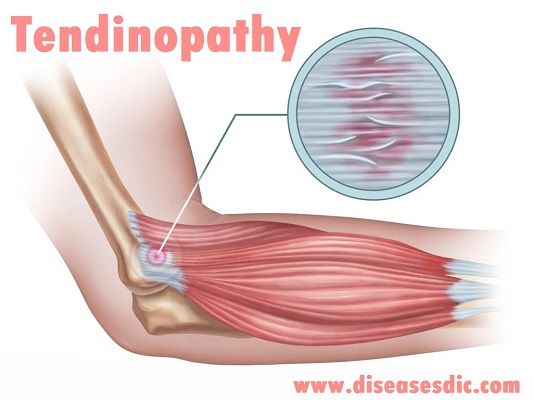
Tendinopathy is the broad term for any tendon condition that causes pain and swelling. Your tendons are rope-like tissues in your body that attach muscle to bone. When your muscles tighten and relax, your tendons and bones move. One example of a tendon is your Achilles tendon, which attaches your calf muscle to your heel bone and causes ankle movement. If you have pain and/or swelling in that area, you might have Achilles tendinopathy. The pain from tendinopathy can interfere with your daily life. For example, it can keep you from playing sports and from doing housework. So, if you have pain or swelling, make sure to contact your healthcare provider for help.
Types of Tendinopathy
Tendinopathy broadly refers to three types of tendon injury, and is often confused with, or used synonymously with them. They are:
- Tendonitis/tendinitis – inflammation of a tendon, usually due to acute injury caused by overuse or repetitive strain.
- Tendinosis – chronic tendon injury with little or no inflammation, involving micro-tears in the affected tendon. Tendinosis causes long-term pain and is degenerative.
- Paratenonitis – inflammation of the outer sheath (paratenon) that surrounds certain tendons, such as the Achilles. There is some debate as to whether this should be considered separate from tendonitis.
All of these conditions increase the risk of a more serious tendon tear, or rupture.
Epidemiology
Tendon injury and resulting tendinopathy are responsible for up to 30% of consultations to sports doctors and other musculoskeletal health providers. Tendinopathy is most often seen in tendons of athletes either before or after an injury but is becoming more common in non-athletes and sedentary populations. For example, the majority of patients with Achilles tendinopathy in a general population-based study did not associate their condition with a sporting activity. In another study the population incidence of Achilles tendinopathy increased sixfold from 1979–1986 to 1987–1994. The incidence of rotator cuff tendinopathy ranges from 0.3% to 5.5% and annual prevalence from 0.5% to 7.4%.
Stages of Tendinopathy
Tendinopathy has three different stages:
- Reactive tendinopathy
- Tendon disrepair
- Degenerative tendinopathy
It’s best to think of these stages as a continuum rather than three distinct phases.
Reactive tendinopathy
It is a short-term adaptation to overload that thickens the tendon, reduces stress and increases stiffness. The tendon has the potential to revert to normal if the overload is sufficiently reduced or if there is sufficient time between loading sessions” Expert physiotherapist thought this reaction involved inflammation but we now understand this is not the case. The tendon does swell but this is due to movement of water into the tendon matrix and not inflammatory products. A key feature of a reactive tendon is that structurally it remains intact and there is minimal change in collagen integrity.
Tendon disrepair
Tendon disrepair describes the attempt at tendon healing, similar to reactive tendinopathy but with greater matrix breakdown. There may be an increase in vascularity and associated neuronal ingrowth. Some reversibility of the pathology is still possible with load management and exercise to stimulate matrix structure.
Degenerative tendinopathy
Degenerative tendinopathy involves areas of cell death due to apoptosis [planned cell death], trauma or tenocyte [tendon cell] exhaustion. As a result, areas of acellularity have been described, and large areas of the matrix are disordered and filled with vessels, matrix breakdown products and little collagen. There is little capacity for reversibility of pathological changes at this stage.
Pathophysiology
Recent data have demonstrated that overuse tendon injuries are not caused by persistent inflammation. The term tendinopathy is commonly used for overuse tendon injuries in the absence of a pathologic diagnosis and describes a spectrum of diagnoses involving injury to the tendon (e.g., tendinitis, peritendinitis, tendinosis). These overuse injuries are most likely to occur when the mode, intensity, or duration of physical activity or athletic training changes in some way. A period of recovery is necessary to meet the increased demands on the tissues; inadequate recovery is thought to lead to breakdown at the cellular level.
A normal response to tendon injury consists of inflammation (i.e., tendinitis) followed by deposition of collagen matrix within the tendon and remodelling (i.e., tendinosis). However, a failed healing response may occur because of ongoing mechanical forces on the tendon, poor blood supply, or both. The tendon undergoes microscopic changes, including fibrin deposition, neovascularization, reduction in neutrophils and macrophages, and an increase in collagen breakdown and synthesis. The resultant tissue consists of a disorganized matrix of hypercellular, hyper-vascular tissue that is painful and weak.
Anatomy of tendon
Causes of Tendinopathy
Overexertion is usually the cause of tendinopathy. Some other causes may include:
- Deposition of calcium in the tendons, also known as calcific tendinopathy
- The development of bone spurs
- Excess jumping or running
- Exercising on hard surfaces
- Holding sporting equipment incorrectly or using unsuitable equipment
- Lifting heavy weights
- Not warming up before exercising or lifting
- Intense physical activity, especially if it is repetitive
- Failing to allow for recovery time
- Working out in the cold
- Having obesity or overweight
- Having flat feet or bowed legs, which causes strain on the tendons
Symptoms of Tendinopathy
Symptoms of tendinopathy may differ in every patient. However, there are some common symptoms associated to the condition. The most prominent amongst these are:
- Pain in the front of your shoulder
- Shoulder pain when reaching behind your back
- Inflammation (tendonitis)
- Shoulder pain when lifting your arm
- Loss of range of motion
- Shoulder pain at night when sleeping on your injured side
- “Clicking” sound when you raise your arm
- Shoulder pain that is worse with use
- Shoulder weakness
- Shoulder stiffness
Risk factors
Risk factors can be intrinsic or extrinsic:
Intrinsic
- Genetic: strongest association with COL5A1, TNC, MMP3and ESRRA
- Sex: increased in female
- Age: increases with age
- Medications, e.g., fluoroquinolones, local and systemic glucocorticoids
- Metabolic, e.g., obesity, type 2 diabetes mellitus, dyslipidaemia, hypercholesterolemia
- Poor muscle strength
Extrinsic
- Excessive tendon beyond tendon capacity, in particular, activities with a high-energy storage component (e.g., jumping in basketball, kicking sports)
- Amount of loading (e.g., increased training time, overuse)
- Change in loading
- “Abusive loading” (i.e., unaccustomed activity) in non-active individuals
- Impingement
- Occupations with high force and/or repetitive activities, e.g., hospitality, factory work, construction, surgeons
Common area of tendinopathy appearance
Complications
Complications with tendinopathy can include the following:
- Contractures of the tendon, with reduced tendon liability
- Tendon adhesions
- Atrophy of muscles
- Loss of functionality, even up to and including disability
Tendinopathy Diagnosis
To diagnose a tendon injury (also known as tendinopathy), your doctor will review your medical history and daily activities and conduct a physical examination to check your overall health, areas of pain and tenderness, and range of motion and strength. Your examination may also include checking your nerve function (feeling and reflexes) and blood circulation (pulses).
If your symptoms are related to use of a tool or sports equipment, your doctor may want you to demonstrate how you use it. If your medical history and physical examination point to a tendon injury, you will probably not need more testing.
If your symptoms are severe or have not improved with treatment, more tests may be helpful. These may include:
- X-rays, which can show any bone-related problems or calcification in tendons or joint structures.
- MRI (magnetic resonance imaging), which can show small tears and areas of tendon, ligament, cartilage, and muscle injury.
- Ultrasound, which can show thickening, swelling, or tears in soft tissues such as the bursae and tendons.
Tendinopathy treatment
The treatment for your tendinopathy depends on the type you have. The treatments for tendinosis aren’t the same as the treatments for tendinitis. Treatment also depends on which tendon is bothering you. The common treatments for tendinosis include:
Ice: Applying ice wrapped in a damp tea towel to the tendon helps reduce pain. Apply for a maximum of 20 minutes, 4 times a day, or after exercise.
Simple painkillers: Paracetamol or anti-inflammatories such as ibuprofen or diclofenac.
Relative rest: You can help to maintain your fitness using different forms of exercise that rest your Achilles tendon, such as swimming, cycling, aqua jogging (running in water). Stretching your calf muscles:
Eccentric exercise program: This particular type of controlled exercise helps your swollen Achilles tendon return to normal and forms the main component of the rehabilitation programme.
Physiotherapy:
This may involve several different treatment options including:
- Manual techniques
- Specific exercises
- Stretches
Other treatments can be considered if these treatments fail. If this happens, your physiotherapist or doctor will discuss them with you. Options include:
- Podiatry referral for assessment for shoe inserts
- High Volume Injection (an injection of saline and anaesthetic into the area around the tendon)
- Autologous Blood Injection (an injection of your own blood into the damaged tendon, to encourage healing)
- Dry needling (this is similar to acupuncture)
- GTN patches (glyceryl trinitrate)
- Surgery
Up-to-date evidence suggests that steroid injections are not the best treatment option; therefore, we do not recommend their use.
Prevention of Tendinopathy
To minimise reinjuring your tendon, you may require some long-term changes to your exercise activities. These should be discussed with your physiotherapist. Some factors that could influence your tendinopathy risk include:
- Altering your sport/activities or your technique
- Regular prevention exercises.
- Closely monitoring and recording your exercise loads. Discuss your loading with your physiotherapist and coach. They will have some excellent tips.
- Always take time to warm up before and cool down / stretch after you exercise.