Overview of Sciatica
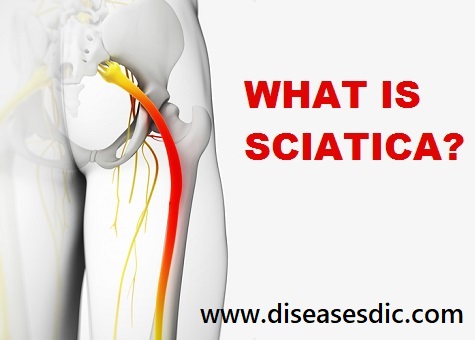
Sciatica is a pain in the lower extremity resulting from irritation of the sciatic nerve. The pain of sciatica is typically felt from the low back (lumbar area) to behind the thigh and can radiate down below the knee. The sciatic nerve is the largest nerve in the body and begins from nerve roots in the lumbar spinal cord in the low back and extends through the buttock area to send nerve endings down the lower limb. Radiculopathy is sometimes referred to as sciatic nerve pain.
Sciatica nerve pain regions
Pregnancy
Although sciatica-like pain can be a problem during pregnancy; an estimated 50–80 percent of women have back pain during pregnancy. Hormones produced during pregnancy, such as relaxin, cause ligaments to loosen up and stretch, which can potentially cause back pain in some women. However, sciatica due to a herniated disk is no more likely during pregnancy.
Types of Sciatica pain
There are two types of sciatica
Neurogenic
In Neurogenic sciatica the pain is caused by compression of the sciatic nerve or smaller nerve roots that form it, symptoms can vary in severity due to the amount of pressure on the nerve. This can be caused by a variety of problems, from bulging discs to tight muscles.
The discs between the vertebra can bulge, herniate or sequestrate (burst) causing direct pressure on the nerves leaving the spine. Pressure directly onto the spinal cord from within the spine can also compromise the function of the sciatic nerve. Tight muscles through the buttocks and top of the legs can also irritate and put pressure on the sciatic nerve.
In most of these cases, the leg pain is worse than the back pain and described as a sharp, burning, shooting pain. It is often associated with a feeling of numbness, pins, and needles, hot and cold sensation and muscle weakness.
With neurogenic sciatica, there are usually abnormal neurological exam findings such as a loss the normal reflexes, muscle weakness, and sensory changes.
Referred
Referred Sciatica is a pain due to a muscle and joint problem in the spine and pelvis, it can mimic sciatica and it is important to determine the cause of your pain. Referred pain is usually dull and achy but can also be sharp in nature. It does not usually cause a feeling of ‘pins and needles’, hot and cold sensation, and numbness or muscle weakness.
In some cases, the pain is worse in the back than it is in the leg and doesn’t usually have a shooting quality to it. Abnormal neurological findings, such as reflex changes, objective weakness, and sensory changes, are unlikely to be present.
Pathophysiology
Sciatica, pain along the sciatic nerve, which runs from the lower back down the legs. Sciatica often develops following an unusual movement or exertion that places a strain on the lumbar portion of the spine, where the nerve has its roots, either immediately or after an interval of several hours to a few days.
Researchers have identified a genetic mutation that significantly increases the risk of the condition. The pain of sciatica may become more severe with coughing, sneezing, and flexion of the neck. It is relieved by positions that minimize traction on the sciatic nerve; for this reason, a person with sciatica tends to walk with the affected leg bent at the knee and externally rotated at the hip.
Anatomy of Sciatica Nerve
Sciatica is commonly associated with the rupture of a portion of an intervertebral disk into the spinal canal. It may also develop as a symptom of some local compressive lesion, or it may indicate a more generalized disorder involving the peripheral nerves. Most cases, including those in which the nerve is displaced by a protruding disk, can be treated effectively by bedrest on a firm mattress for several days to a few weeks. In some instances, however, surgical decompression of the nerve is necessary in order to prevent repeated attacks of disabling pain or to relieve weakness and sensory loss in the leg.
What Causes Sciatica?
Sciatica is caused by irritation of the root(s) of the lower lumbar and lumbosacral spine.
Additional common causes of sciatica include:
- Lumbar spinal stenosis (narrowing of the spinal canal in the lower back)
- Degenerative disc disease (breakdown of discs, which act as cushions between the vertebrae)
- Spondylolisthesis (a condition in which one vertebra slips forward over another one)
- Pregnancy
- Muscle spasm in the back or buttocks
- Piriformis syndrome is an uncommon cause of sciatica. The piriformis is a muscle that lies deep underneath the gluteal muscles of the buttocks. The function of the piriformis muscle is to externally rotate and stabilize the hip. The sciatic nerve passes directly underneath the piriformis. Piriformis syndrome occurs when the piriformis muscle becomes tight, goes into spasm, or swells. When this happens it compresses the sciatic nerve beneath it.
- Bony growths (osteophytes): Bone spurs or osteophytes are bony outgrowths on the edges of joints. Bone spurs form where cartilage is worn away (for example in osteoarthritis) and bone is rubbing on bone. Bone spurs are not painful in themselves, but unfortunately, the bone spurs can rub on nearby bone or nerves, causing problems. In the spine, bone spurs can intrude into space normally reserved for the nerves, thus causing sciatica.
Other things that may make your back pain worse include being overweight, not exercising regularly, wearing high heels, or sleeping on a mattress that is too hard or too soft.
Risk factors for sciatica include:
- Age-related changes in the spine, such as herniated disks and bone spurs, are the most common causes of sciatica.
- By increasing the stress on your spine, excess body weight can contribute to the spinal changes that trigger sciatica.
- A job that requires you to twist your back, carry heavy loads or drive a motor vehicle for long periods might play a role in sciatica, but there’s no conclusive evidence of this link.
- Prolonged sitting. People who sit for prolonged periods or have a sedentary lifestyle are more likely to develop sciatica than active people are.
- This condition, which affects the way your body uses blood sugar, increases your risk of nerve damage.
What are the symptoms of sciatica?
Common symptoms of sciatica include
- Lower back pain
- Pain in the rear or leg that is worse when sitting
- Hip pain
- Burning or tingling in the leg
- Weakness, numbness, or difficulty moving the leg or foot
- Constant pain on one side of the rear
- A shooting pain that makes it difficult to stand up
What are the complications of sciatica?
Complications due to sciatica are rare. If they do occur they can include:
- Permanent nerve damage
- Loss of feeling in the affected leg
- Weakness in the affected leg
- Loss of bowel or bladder function
Diagnosis and test for Sciatica
Physical exam
During the physical exam, your doctor may check your muscle strength and reflexes. For example, you may be asked to walk on your toes or heels, rise from a squatting position and, while lying on your back, lift your legs one at a time. Pain that results from sciatica will usually worsen during these activities.
Imaging tests
Many people have herniated disks or bone spurs that will show up on X-rays and other imaging tests but have no symptoms. So doctors don’t typically order these tests unless your pain is severe, or it doesn’t improve within a few weeks.
- X-ray. An X-ray of your spine may reveal an overgrowth of bone (bone spur) that may be pressing on a nerve.
- This procedure uses a powerful magnet and radio waves to produce cross-sectional images of your back. An MRI produces detailed images of bone and soft tissues such as herniated disks. During the test, you lie on a table that moves into the MRI machine.
- CT scan. When a CT is used to image the spine, you may have a contrast dye injected into your spinal canal before the X-rays are taken – a procedure called a CT myelogram. The dye then circulates around your spinal cord and spinal nerves, which appear white on the scan.
- Electromyography (EMG). This test measures the electrical impulses produced by the nerves and the responses of your muscles. This test can confirm nerve compression caused by herniated disks or narrowing of your spinal canal (spinal stenosis). What are the treatments for sciatica?
How Sciatica is treated?
We will look at treatments for acute and chronic sciatica individually:
Acute sciatica treatments
Most cases of acute sciatica respond well to self-care measures, which include:
- Over-the-counter painkillers such as ibuprofen, which are also available to buy online.
- Exercises such as walking or light stretching.
- Hot or cold compression packs help to reduce pain. They are available to purchase online. It is often helpful to alternate between the two.
Not all painkillers are suitable for everyone; individuals should be sure to review options with their doctor.
Chronic sciatica treatments
Treatment of chronic sciatica usually involves a combination of self-care measures and medical treatment:
- Physical therapy
- Cognitive behavioral therapy (CBT) – helps manage chronic pain by training people to react differently to their pain
- Painkillers
Surgery
Surgery may be an option if symptoms have not responded to other treatments and continue to intensify. Surgical options include:
- Lumbar laminectomy – widening of the spinal cord in the lower back to reduce pressure on the nerves.
- Discectomy – partial or entire removal of a herniated disk.
Depending on the cause of sciatica, a surgeon will go over the risks and benefits of surgery and be able to suggest a suitable surgical option.
Rehabilitation
- Your doctor may give you exercises to strengthen your back. It is important to walk and move while limiting too much bending or twisting. It is acceptable to perform routine activities around the house, such as cooking and cleaning.
- Following treatment for sciatica, you will probably be able to resume your normal lifestyle and keep your pain under control. However, it is always possible for your disk to rupture again.
Can sciatica be prevented?
Some sources of sciatica are not preventable, such as degenerative disc disease, back strain due to pregnancy, and accidental falls.
Although it might not be possible to prevent all cases of sciatica, you can take steps to protect your back and reduce your risk.
- Practice proper lifting techniques. Lift with your back straight, bringing yourself up with your hips and legs, and holding the object close to your chest. Use this technique for lifting everything, no matter how light.
- Avoid/ stop cigarette smoking, which promotes disc degeneration.
- Exercise regularly to strengthen the muscles of your back and abdomen, which work to support your spine.
- Use good posture when sitting, standing, and sleeping. Good posture helps to relieve the pressure on your lower back.
- Avoid sitting for long periods.