Milroy’s Disease – Definition
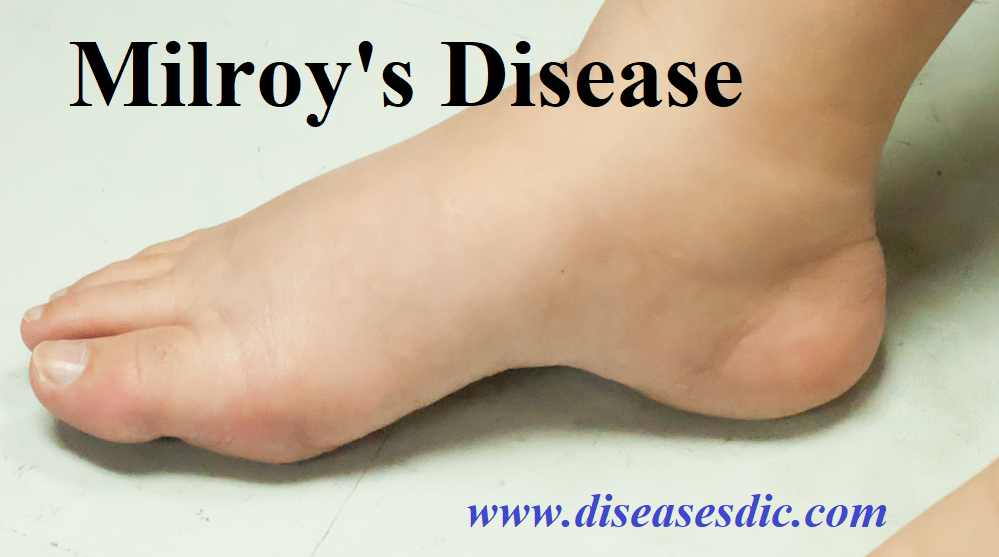
Milroy’s Disease is a condition that affects the normal function of the lymphatic system. The lymphatic system produces and transports fluids and immune cells throughout the body. Impaired transport with an accumulation of lymph fluid can cause swelling (lymphedema). Individuals with Milroy disease typically have lymphedema in their lower legs and feet at birth or develop it in infancy. The lymphedema typically occurs on both sides of the body and may worsen over time.
Milroy disease is associated with other features in addition to lymphedema. Males with Milroy disease are sometimes born with an accumulation of fluid in the scrotum (hydrocele). Males and females may have up slanting toenails, deep creases in the toes, wart-like growths (papillomas), and prominent leg veins. Some individuals develop non-contagious skin infections called cellulitis that can damage the thin tubes that carry lymph fluid (lymphatic vessels). Episodes of cellulitis can cause further swelling in the lower limbs.
How is Milroy’s Disease inherited?
Milroy disease is inherited in an autosomal dominant manner. This means that having one changed (mutated) copy of the responsible gene in each cell is enough to cause symptoms of the condition. When a person with an autosomal dominant condition has children, each child has a 50% (1 in 2) chance to inherit the mutated copy of the gene.
Most people with Milroy disease have an affected parent, but some cases are due to new mutations that occur for the first time in the affected person. About 10-15% of people with a mutation in the responsible gene do not develop features of the condition. This phenomenon is called reduced penetrance.
Causes of Milroy’s disease
Mutations in the FLT4 gene cause some cases of Milroy disease. The FLT4 gene provides instructions for producing a protein called vascular endothelial growth factor receptor 3 (VEGFR-3), which regulates the development and maintenance of the lymphatic system. Mutations in the FLT4 gene interfere with the growth, movement, and survival of cells that line the lymphatic vessels (lymphatic endothelial cells). These mutations lead to the development of small or absent lymphatic vessels. If lymph fluid is not properly transported, it builds up in the body’s tissues and causes lymphedema. It is not known how mutations in the FLT4 gene lead to the other features of this disorder.
Many individuals with Milroy disease do not have a mutation in the FLT4 gene. In these individuals, the cause of the disorder is unknown.
Risk factors of Milroy’s disease
The following are the risk factors for Milroy disease:
- Age and sex
- Family history
- Immune system problems
- Infections
- Previous cancers
- Precursor conditions (non-cancerous conditions of lymphocytes)
Signs and Symptoms
The main symptom is swelling of the lower leg (usually limited below the knee). It affects both legs but the right leg tends to be worse. Infant males may have a swollen scrotum (hydrocele). It is important to note that swelling can occur at any site where the lymphatic vessels are abnormally small or absent. Gravity does play a role in the presentation as the fluid accumulates in the lowest parts of the body, like the legs. The swelling is generally soft and pitting. Certain affected areas may be hard with a “woody” feeling due to fibrosis. The swollen area may be warm to touch.
Cellulitis is common in patients with Milroy disease. The swelling in these cases is worse than just the disease on its own, there is usually redness of the skin, heat, and tenderness. An oozing wound may also be present.
Apart from these symptoms, there may also be:
- Up slanting toenails
- Enlarged leg veins
- Wart-like growths (papillomas)
- Thickened skin with deep creases
Complications
Milroy disease is rarely associated with significant complications.
- The degree of edema sometimes progresses, but in some cases can improve (particularly in early years).
- Complications of lymphedema may include recurrent bouts of cellulitis and/or lymphangitis, bacterial and fungal infections, deep venous thrombosis, functional impairment, cosmetic embarrassment, and amputation.
- Complications following surgery are common. It has also been reported that people with chronic lymphedema for many years may have a significantly higher risk to develop lymphangiosarcoma (a type of angiosarcoma). This type of tumor is highly aggressive and has a very poor prognosis.
Tests and Diagnosis
Milroy disease is often diagnosed at birth or shortly thereafter. Typically the lower leg is edematous (swollen) and male babies may be born with a swollen scrotum (hydrocele) as well. In order to confirm the diagnosis, various tests need to be done. Genetic testing is not necessary because not every patient with Milroy disease has a mutation in the FLT4 gene and not every person with this genetic mutation has Milroy disease.
Scans
Traditional imaging tests are useful for excluding other possible causes of lymphedema but the following investigations are more specific for Milroy disease:
- Lymphoscintigraphy is an investigation where images are captured after the injection of radioactive particles (radiotracers).
- Fluorescence microlymphography uses a fluorescent material to provide images of very small vessels of the lymphatic system (microlymphatics).
Both these studies may reveal abnormally small or absent lymphatic vessels. An MRI (magnetic resonances imaging) scan may also be useful in identifying lymphedema.
Biopsy
A punch biopsy is where a sample of tissue is collected to be examined under a microscope. The examination reveals the lymphatic vessels are absent although in late stages there may be signs of abnormally dilated vessels. Fibrosis is also detected on examination of the biopsy sample.
Treatment and medication
Management is typically conservative and usually successful in most people. The goal of treatment is to reduce swelling and prevent complications. Management of lymphedema should be guided by a lymphedema therapist. Complete decongestive therapy (CDT) may be used for manual lymph drainage combined with compression bandaging, skincare, exercise, and well-fitted compression garments. Some improvement is usually possible using these methods. Various surgical techniques (to reduce swelling by creating new pathways for lymphatic fluid to flow) have been tried, but with limited success.
To prevent cellulitis, foot infections (such as athlete’s foot) should be treated promptly and prevented, and prophylactic antibiotics may be needed in recurrent cases. When possible, people with Milroy disease should try to avoid wounds to swollen areas, long periods of immobility, medications that can cause increased leg swelling (such as calcium channel-blocking drugs and non-steroidal anti-inflammatory drugs), and excessive salt intake which can cause fluid retention.
Medication
There is no medication for Milroy disease itself but various drugs may be useful for the complications. Antibiotics are used to treat infections in cellulitis, a common complication in Milroy disease. Sometimes antibiotic injections can be administered monthly to prevent infection in high-risk patients. Anticoagulants may also be prescribed on an ongoing basis.
Prognosis of Milroy’s Disease
- MD does not normally affect life expectancy. Patients may have recurrent streptococcal cellulitis and lymphangitis, with subsequent hospitalizations for antibiotic therapy.
- A rare complication is the appearance of lymphangiosarcoma or angiosarcoma in patients with persistent lymphedema.
- Some patients may develop protein-losing enteropathy and visceral involvement. Chylous ascites and chylothorax rarely occur.